How to Prevent Flu and COVID-19 Infections and Complications
Unless you're a hermit living alone in the woods, you face up to a 25% chance of catching the flu this year, regardless of vaccination status. Up to 70% of infected individuals will recover within a week, while the rest may experience complications of varying severity.
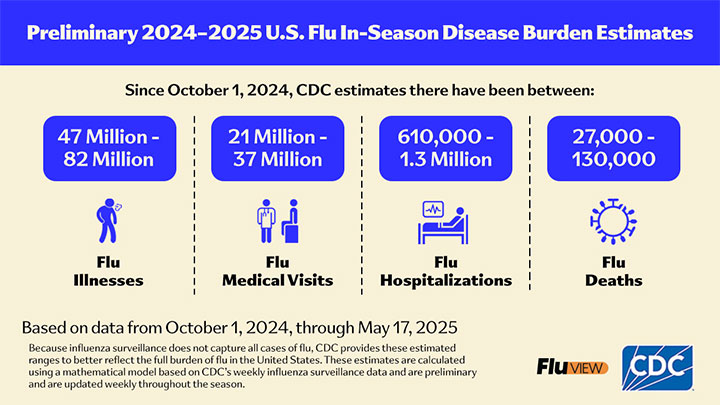
This chart from the U.S. Centers for Disease Control and Prevention (CDC) shows the extent of the flu epidemic during the 2024–2025 flu season [link]:
The Odds of Getting Infected and the High Price to Pay
If you're not worried enough already, let me share a few more statistics about what to expect from this year's flu season:
-
An adult's chance of getting symptomatic flu in the 2025-26 season is up 25%. Your risks increase exponentially if you or your family members commute to work on public transportation, interact with the public at work, or have school-age children.
-
Adults over 50 are disproportionately affected by severe complications from these conditions, are more likely to be hospitalized, and have a higher risk of dying from pneumonia or other related issues.
-
The national average hospital cost per day is about $3,025. The typical insured out-of-pocket cost for a three-day stay is $1,300–$2,500. The cost of lost income or wages depends on your occupation and employer.
-
Recovery from a complicated flu often involves lingering symptoms like severe fatigue and a cough that can last two weeks or more, and may delay a full return to work even after the initial fever and acute symptoms have gone.
The combined risks of infection, long-term side effects, and financial loss are too high to rely on luck alone.
If COVID Is Bad Enough, Long COVID Is Far Worse
The chart above doesn't include COVID-19 infections. Over the period from April 27, 2025 to April 25, 2026, cumulative hospitalizations for COVID are projected at about 648,000 and deaths around 40,000, with the majority of severe outcomes occurring in individuals aged 65 and older [link].
People who don't recover from COVID within a week are confronted with long COVID, which is a chronic condition following infection and lasting for months or years:
-
Among adults who have ever had COVID, around 29% have experienced long COVID at some point, with about 1 in 10 currently having it. This prevalence has been relatively stable since 2023.
-
In the United States, approximately 7% to 8% of all adults currently report having long COVID symptoms, translating to about 17 million individuals.
-
Long COVID is more common among women, middle-aged individuals, and those who had severe symptoms initially.
The most common symptoms include fatigue, brain fog, shortness of breath, headaches, muscle and joint pain, chest pain, palpitations, dizziness, sleep problems, cough, loss or change in smell and taste, gastrointestinal issues like diarrhea and stomach pain, depression, anxiety, hair loss, skin rashes, and more than two hundred others. Similar symptoms have been reported for non-COVID flu, but they don't last as long.
The Unprepared Pay Thrice
By paying thrice, I mean: (1) getting infected in the first place, (2) needing hospitalization after it, and (3) developing long-term side effects. Dying becomes somebody else's problem, so I'm not including it in this math.
Flu hospitalizations and complications result from an interplay between the virus's impact and your immune and metabolic state. Chronic inflammation, nutrient deficiencies, medication side effects, and delayed recovery mechanisms all increase the risk of severe outcomes.
Knowing these facts, it makes sense to eliminate, as much as possible, the primary factors behind flu-related complications and mortality.
You're likely familiar with Pareto's rule, which states that 20% of the effort yields 80% of the results. In this article, I will explore the four key pillars of flu and COVID-19 prevention that represent those proverbial 20% with the greatest return on your efforts. Respectively, they are:
-
Not getting infected in the first place;
-
Reducing chronic inflammation;
-
Restoring the protective properties of the gastrointestinal tract, and…
-
Strengthening the immune system.
Here we go, starting from the most obvious and reliable option, which is…
1. Not Getting Infected in the First Place
In a controlled "human challenge" study of COVID-19, healthy volunteers were intentionally exposed to the virus under identical conditions, but not everyone became infected, even though all received the same viral load exposure:
To our surprise, we found that, despite all the volunteers being carefully exposed to the exact same dose of the virus in the same manner, not everyone ended up testing positive for COVID. [link]
It's also a well-established fact that many children and adults living in the same households, as well as healthcare workers regularly exposed to infected patients, do not get sick, which is clear evidence that individual resistance varies dramatically.
To prevent exposure from turning into an infection in the first place, I recommend focusing on the next three pillars, starting with reducing chronic inflammation, because healthy respiratory and digestive membranes serve as biological barriers that block viruses you inhale through the nose and those you swallow with saliva through the mouth.
Of course, this approach doesn't rule out other common-sense protective measures, such as dressing appropriately to avoid cold exposure, wearing a mask in public places, cleansing hands with sanitizer, and not touching your face with contaminated hands.
2. Reduce Chronic Inflammation
Reducing chronic inflammation also means addressing underlying respiratory conditions such as chronic sinusitis, rhinitis, bronchitis, asthma, and chronic obstructive pulmonary disease (COPD) that keep your respiratory pathways inflamed and vulnerable.
If you get hyperinsulinemia under control, your risk of pneumonia, complications, and long COVID will drop by 20–30% in my estimation. The risk of infection itself will fall even further because reduced inflammation in the respiratory and digestive tracts restores the natural defenses of their mucosal linings.
When these tissues remain swollen and congested, their mucosal defenses weaken, allowing viruses and bacteria to penetrate deeper into the airways and lungs, greatly increasing the risk of infection and complications.
Chronic inflammation doesn't happen by accident. It is related to pre-existing conditions that can impair immune response and exacerbate flu severity. Influenza infection itself triggers systemic inflammation that can remain for weeks, worsening chronic conditions and increasing risks of complications like heart attacks or strokes.
Persistently elevated insulin and blood sugar are the most common drivers of chronic inflammation. Even modest glucose fluctuations keep tissues in a constant state of low-grade inflammation.
Reducing meal frequency to two (best) or a maximum of three meals per day, eliminating between-meal snacks, keeping carbohydrate intake moderate, and eliminating sweets stabilizes glucose and insulin levels and cuts inflammatory cytokine activity within weeks.
The strongest triggers of insulin secretion are:
-
Sweetness from sugar and sweetened foods and drinks. Fruits, juices, snacks, candies, cookies, cakes, ice cream, soft drinks, and sweet alcoholic beverages all raise insulin. The sugar in fruit is just as harmful as table sugar because, once inside the body, it's broken down into the same molecules — glucose, fructose, and galactose — which trigger insulin release all the same.
Non-sweet carbohydrates in moderation, such as bread, rice, pasta, and potatoes, are gradually converted to glucose by digestive enzymes, but they do not raise insulin levels as sharply as naturally sweet carbohydrates or foods with added sugars.
-
Sweetness from artificial and natural sweeteners. Artificial sweeteners (aspartame, sucralose, saccharin, acesulfame potassium) and "'natural" ones (stevia, erythritol, xylitol, monk fruit extract) can be just as harmful as sugar.
The body begins secreting insulin in response to sweetness long before sweet food reaches the small intestine. They can be even more harmful, because with real sugar, cells at least absorb glucose in response to insulin, which then suppresses further secretion — but with artificial sweeteners, that feedback loop doesn't occur.
-
Alcohol. It is the most harmful trigger because it blocks normal sugar metabolism. This forces the pancreas to pump out large amounts of insulin to prevent hypoglycemia (low blood sugar). The sensation of drunkenness is, in fact, a manifestation of low blood sugar. This reaction also explains why alcohol causes intense sugar cravings and stimulates appetite.
-
Diabetes medications that stimulate insulin secretion by forcing the pancreas to release more insulin. They include sulfonylureas (glipizide, glyburide, glimepiride) and meglitinides (repaglinide, nateglinide). While they temporarily lower blood sugar, they also keep insulin chronically elevated, reinforcing the very inflammatory state that drives metabolic decline.
-
Diabetes medications that lower blood sugar through other mechanisms. Drugs such as metformin, SGLT2 inhibitors (Ardiance, Invokana, Farxiga, Steglatro, Brenzavvy), and GLP-1 receptor agonists (Ozempic, Wegovy, Zepbound) don't raise insulin directly, but they come with their own costs. Each can provoke side effects that may amplify inflammation even more than elevated insulin itself. In many patients, these secondary effects prolong fatigue, impair recovery, and weaken resistance to infection.
-
All-meat and carnivore diets are often promoted as "'low-carb" or "'insulin-friendly," yet they provoke substantial insulin release because protein itself, particularly from meat and dairy, strongly stimulates the pancreas. In practice, these diets can keep insulin elevated almost continuously while depriving the body of magnesium, potassium, and antioxidants needed to control inflammation. The short-term weight loss some people see comes from glycogen depletion and dehydration, not improved metabolic balance.
I realize this point may trigger immense hate from the carnivore community, but I didn't make any of this up. Here are academic peer-reviewed studies regarding this physiological phenomenon:
-
Nuttall FQ, Gannon MC. Plasma glucose and insulin response to macronutrients in nondiabetic and NIDDM subjects. Diabetes Care. 1991;14(9):824-838.
Protein stimulates insulin secretion, and this is relatively more prominent in people with NIDDM [Type 2 diabetes – KVM]. [link]
-
Van Loon LJ et al. Plasma insulin responses after ingestion of different amino acid or protein mixtures with carbohydrate. Am J Clin Nutr. 2000;72(1):96-105
Insulin responses are positively correlated with plasma leucine, phenylalanine, and tyrosine concentrations [These are amino acids – KVM]. A mixture of wheat protein hydrolysate, free leucine, phenylalanine, and carbohydrate can be applied as a nutritional supplement to strongly elevate insulin concentrations. [link]
-
Holt SH et al. An insulin index of foods: the insulin demand generated by 1000-kJ portions of common foods. Am J Clin Nutr. 1997;66(5):1264-1276.
However, protein-rich foods and bakery products (rich in fat and refined carbohydrate) elicited insulin responses that were disproportionately higher than their glycemic responses [effect on blood sugar – KVM]. [link]
Please don't misconstrue my observations and recommendations as "what else is left to eat?" I'm not arguing for the exclusion of any particular food group, but for having a balanced diet that includes carbohydrates, fats, and proteins in moderation, while avoiding foods that are outright toxic or harmful.
-
-
Dairy products are strong insulin triggers because they combine lactose (a sugar) with whey protein (a potent insulin stimulator). A glass of milk can raise insulin more than an equal amount of carbohydrate from table sugar.
-
Caffeine and stimulants provoke insulin indirectly by stimulating adrenaline and cortisol, which prompt the liver to release glucose. The pancreas responds by releasing insulin to counteract the spike, often resulting in a post-caffeine crash or sudden hunger.
-
Stress and lack of sleep are among the most powerful non-dietary insulin triggers. Elevated cortisol and adrenaline keep blood sugar high even without food, forcing the pancreas to secrete more insulin to restore balance.
-
Chronic overeating and frequent snacking keep insulin perpetually elevated because every eating event — even a small "'healthy" snack — requires a new insulin response. Without long fasting intervals, the body never gets a break to burn fat or repair tissues.
-
Inactivity makes muscles less responsive to glucose, forcing the pancreas to secrete more insulin for the same amount of carbohydrate. Even a brief walk after meals can lower post-meal insulin levels and inflammation dramatically.
-
Exercise influences insulin in opposite ways depending on its intensity and duration. Moderate, steady activity improves insulin sensitivity and helps clear glucose without large insulin spikes. But intense or prolonged exercise — especially on an empty stomach — can temporarily raise insulin because stress hormones (adrenaline and cortisol) drive glucose release from the liver. The body compensates by secreting insulin to prevent blood sugar from rising too high. In overtrained or undernourished individuals, this can actually worsen inflammation and fatigue instead of improving metabolism.
-
Medications such as corticosteroids, beta-blockers, and antipsychotics can raise insulin either by increasing blood sugar or by directly stimulating pancreatic signaling. Some hormonal contraceptives and antidepressants have similar effects.
As you can see from this list, you can lead a perfectly "'healthy" diet and lifestyle yet keep your body in a constant state of hyperinsulinemia and chronic inflammation — the underlying cause of excessive appetite, sugar cravings, overeating, weight gain, atherosclerosis, hypertension, heart disease, strokes, diabetes, memory loss, dementia, neurological disorders, bone and joint disease, digestive problems, blindness, allergies, suppressed immunity, and, of course, respiratory conditions of all types that open a welcome door to flu, COVID, and pneumonia.
All of the above disorders are the "'symptoms" of metabolic syndrome — a catch-all term for the wide range of side effects that stem from chronically elevated blood sugar and insulin. I'm sure you'd rather not have even one of them.
The other major benefit of normalizing insulin secretion is stress reduction, because insulin is a first-line hormone that regulates the "'fight or flight" response. Elevated insulin keeps the body in a constant state of biochemical alert, driving anxiety, irritability, and poor sleep through its effects on cortisol and adrenaline. When insulin levels stabilize, so do mood, focus, and emotional resilience.
3. Restore the Protective Properties of the Stomach
This section is particularly important for preventing COVID infections because the SARS-CoV-2 virus enters host cells by binding to the ACE2 receptor. These receptors are abundant throughout the gastrointestinal tract, including the stomach, duodenum, ileum, and colon, and allow the virus to invade and replicate within epithelial cells. Symptoms such as diarrhea, nausea, and abdominal pain are common in COVID and reflect active viral replication in the gut, which contributes directly to disease severity and mortality.
Knowing that, the stomach is your first and last barrier between you and the poisons from the outside world. Every virus, bacterium, or fungal spore you swallow along with contaminated food, mucus, or saliva is meant to be destroyed by the stomach's acid before it reaches the intestines or bloodstream. When this defense fails, the digestive tract becomes a highway for infection, inflammation, and autoimmune reactions.
Low stomach acid (hypochlorhydria) is the most common cause of this failure. Contrary to popular belief, acid deficiency — not excess — underlies most cases of indigestion, reflux, bloating, and chronic gastritis. Without sufficient acidity (pH below 2.0), the stomach can't sterilize incoming food or neutralize pathogens from the respiratory tract that are swallowed with mucus during flu or COVID infections.
Here are the primary factors that reduce acidity:
-
Chronic inflammation of the stomach mucosa. Continuous irritation from alcohol, overeating, infections, medications, or autoimmune reactions damages the parietal cells responsible for producing hydrochloric acid. Over time, this leads to atrophic gastritis — a thinned, underperforming mucosa incapable of generating enough acid to digest food or kill pathogens.
-
Dehydration. Too little reduces the volume of gastric secretions and thickens the mucus that protects the stomach lining. Without proper hydration, acids and enzymes become concentrated and poorly regulated — too weak for digestion at first, then too harsh against unprotected tissue. Chronic dehydration also disrupts electrolyte balance, which further impairs acid production.
-
Overhydration. Consuming too much water or fluids after meals dilutes and neutralizes stomach acid, weakens its concentration, and reduces its sterilizing and digestive powers. It's best to drink a moderate amount before and during meals.
-
Low-salt diets. Chloride from dietary salt is the raw material for hydrochloric acid. Restricting sodium for long periods can unintentionally suppress acid production. This is especially common among people on blood-pressure medications or "'heart-healthy" low-sodium diets, which lower stomach acid and impair protein digestion.
-
Alcohol. Drinks suppress the secretion of stomach acid, digestive enzymes, and peristalsis. Food remains in the stomach longer, ferments instead of being digested, and increases the risk of reflux, gastritis, and bacterial overgrowth.
-
Vegetarian diets. Low protein intake reduces the stimulation of gastrin, the hormone that triggers acid secretion. Without adequate protein, the stomach "'forgets" to make acid, leading to incomplete digestion, bloating, and bacterial overgrowth. Many plant foods also buffer acid through their alkaline minerals, further reducing acidity.
-
Eating at the wrong time. Acid secretion follows a circadian rhythm and anticipatory response. Eating late at night or grazing throughout the day disrupts this rhythm, leaving acid levels low when food arrives and causing reflux or heaviness after meals.
-
Jet lag. Disrupted circadian rhythms interfere with the body's normal timing of digestive secretions, including stomach acid. When sleep, daylight exposure, and mealtimes are out of sync, the stomach doesn't produce acid when food arrives and overproduces when it shouldn't. This mismatch leads to poor digestion, reflux, and loss of the stomach's antimicrobial defense, one reason frequent travelers are more prone to gut and respiratory infections.
-
Overeating. Large meals stretch the stomach wall and dilute existing acid with food volume. The resulting pH is too high to activate pepsin, the main enzyme that digests protein. Gas and fermentation from undigested food push acid upward, causing reflux and heartburn.
-
Frequent small meals throughout the day. Constant eating keeps digestion running without pause, forcing the stomach to secrete acid and enzymes almost continuously. Over time, it exhausts the parietal cells and depletes the stomach's ability to produce sufficient acid for main meals. This "'always-on" pattern leads to weak digestion, bacterial overgrowth, and a constant feeling of heaviness or bloating.
-
Snacking between meals. Constant eating prevents the stomach from fully emptying and resetting its pH between meals. This keeps acid secretion irregular and weakens digestion, promoting fermentation and bloating.
-
Weight-loss diets. Severe calorie restriction and low-protein regimens lower gastrin and acid production. Prolonged fasting or undernutrition weakens stomach tone and slows emptying, often mimicking "'too much acid" symptoms and driving people to take unnecessary acid-suppressing drugs.
-
Weight-loss medications. Appetite-suppressing and gastric-slowing drugs (such as GLP-1 receptor agonists) interfere with the feedback that normally stimulates acid secretion. They prolong food retention in the stomach, causing reflux, nausea, and bacterial overgrowth.
-
Antacids, PPIs, and H2 blockers. These drugs directly neutralize or block acid production. Long-term use destroys the stomach's antimicrobial barrier, increasing vulnerability to pneumonia, SIBO, and intestinal infections. Studies show higher rates of respiratory illness in chronic users because swallowed pathogens are no longer neutralized by acid.
-
Allergy medications (antihistamines). Histamine triggers acid secretion. Antihistamines — especially H2 blockers and older allergy drugs — suppress this signal, leading to low acid, poor digestion, and a weakened immune barrier in the upper gut.
-
Drugs that reduce motility. Medications such as sleep aids, antidepressants, anti-anxiety drugs, and certain painkillers suppress the parasympathetic nervous system, which controls digestion. As a result, stomach contractions slow, acid secretion drops, and food stagnates and ferments.
-
Stress. Emotional or physical stress diverts blood flow and energy away from digestion, shutting down acid secretion and gastric motility. In this "'fight-or-flight" state, digestion literally stops, leading to nausea, bloating, or loss of appetite.
-
Intense exercise. Moderate physical activity supports digestion, but strenuous or prolonged exercise — especially before or soon after meals — suppresses acid secretion and slows stomach emptying. The body prioritizes blood flow to muscles over digestion, effectively pausing stomach function.
-
Highly focused work in front of the computer. Intense mental concentration activates the same stress pathways as emotional strain. Blood flow shifts from the stomach to the brain, suppressing acid secretion and peristalsis. Eating while working, reading, or typing leaves the stomach "'half asleep," causing indigestion and post-meal fatigue.
You don't need to memorize this list or fix everything at once. Each of these habits undermines digestion in its own way, but the principle is the same — the stomach can't protect you if it's constantly diluted, suppressed, or out of rhythm.
When gastric acidity is normalized, pathogens that enter through the mouth are neutralized before they reach the intestines or lungs. This single step dramatically reduces the burden of infections, food intolerances, and post-viral complications that stem from gut inflammation.
Just like with hyperinsulinemia, normalizing stomach digestion and protective properties will reduce your risk of complications by another 20% to 30% and will also greatly decrease the risk of COVID infection with the oral and GI tract path.
4. Strengthen Immunity
The last and most important barrier to flu and COVID is your immune system, because it fights infection once the virus has already entered your body. That’s the difference between recovering fully at home versus ending up in a hospital, and between complete recovery versus developing long COVID or other complications.
The immune system has two main components: innate and adaptive.
-
Innate immunity is the defense you are born with. It provides an immediate, non-specific response to infection. It includes physical barriers like the skin and mucous membranes, and immune cells such as macrophages and natural killer (NK) cells that destroy invading pathogens. The innate immune response acts within hours of exposure but lacks memory, so it responds the same way each time a pathogen is encountered.
-
Adaptive immunity (also called acquired) develops over time as you are exposed to infections or vaccines. It takes longer to activate than the innate system, but it has the advantage of memory, providing faster and stronger protection when the same pathogen returns.
Both systems work together to defend the body. This dual design allows immunity to be both fast and precise in its response to infection.
The effectiveness of innate and adaptive immunity depends on a wide range of micronutrients derived from food, water, and supplements. These include:
Vitamin A
Vitamin A is essential for maintaining the integrity of all epithelial tissues of the skin, respiratory tract, digestive tract, and urinary passages, which serve as the body's first physical barrier against pathogens. It supports the production of mucus, the secretion of antibodies, and the activation of white blood cells that target viruses and bacteria.
Deficiency in vitamin A weakens these protective barriers, leading to dry mucous membranes, poor wound healing, and higher susceptibility to respiratory and gastrointestinal infections. During or after a viral illness, low vitamin A levels delay recovery and increase the risk of secondary bacterial complications.
The best dietary sources include liver, cod liver oil, butter, egg yolks, and full-fat dairy. Plant-based sources such as carrots and leafy greens provide beta-carotene, a precursor to vitamin A, but its conversion to active retinol is inefficient, especially in older adults and individuals with thyroid or gut disorders.
Supplementation with 2,500 to 5,000 IU daily is typically safe and effective for immune support during flu season.
Vitamin A (5,000 IU / 1,500 mg) is included in the Coenzymated Once Daily Multi formula that I recommend to my clients and take daily myself.
Vitamin D
Vitamin D regulates both innate and adaptive immunity. It enhances the pathogen-fighting power of macrophages and natural killer cells while reducing excessive inflammation that can damage tissues. Low vitamin D levels are strongly associated with higher rates of respiratory infections, severe COVID outcomes, and slower recovery from viral illnesses.
The effectiveness of vitamin D is one of the reasons why regions with abundant sunlight, such as Hawaii, consistently report lower rates of infection, hospitalization, death, and long COVID.
However, more is not better. Excessive vitamin D intake can cause mineral loss, kidney stones, and electrolyte imbalances. For most adults, 1,000 IU per day is sufficient to maintain healthy levels.
How to take: Vitamin D (1,000 IU / 25 mcg) is included in the Coenzymated Once Daily Multi formula.
Vitamin E
Vitamin E protects the membranes of cells and mitochondria from the damage caused by unstable oxygen compounds formed
during infection and inflammation. This protection helps immune cells — particularly T cells and macrophages — remain
functional and responsive during viral and bacterial attacks.
Deficiency in vitamin E weakens immune
responsiveness, slows recovery from infection, and increases the risk of chronic inflammatory and degenerative
conditions. Adequate intake also helps maintain lung tissue integrity and reduces the severity of respiratory
infections in older adults and those with chronic illness.
Natural sources include nuts, seeds, avocados,
olives, and unrefined vegetable oils such as sunflower, safflower, and olive oil. However, the vitamin E content of
most processed oils and packaged foods is severely degraded by heat and exposure to air.
How to take: Vitamin E (30 I.U. / 20 mg) is included in the Coenzymated Once Daily Multi formula. I take an additional 400 I.U. of Natural Vitamin E to account for my age and its other benefits that I address on the respective pages.
Vitamin C
Vitamin C is essential for both the innate and adaptive immune response. It supports the production and function of white blood cells, enhances antibody formation, and protects tissues from oxidative damage caused by inflammation. During infections, the body's demand for vitamin C rises sharply because it is used up in neutralizing free radicals generated by the immune response.
The idea that you can get all the vitamin C you need from orange juice, fruits, and vegetables is preposterous for several reasons.
-
First, vitamin C is highly unstable — it oxidizes rapidly when exposed to air, light, or heat. By the time most fruits or juices reach your table, much of their vitamin C content is already gone.
-
Second, the actual concentration of vitamin C in most fruits and vegetables is modest. You would need to consume several pounds of fresh produce daily to reach even the minimum effective dose needed to support immune defenses during infection.
-
Third, modern agricultural and storage practices have significantly reduced the vitamin content of produce. Long transport times, refrigeration, and cooking further degrade vitamin C, leaving little more than traces in what appears to be a "healthy" diet.
-
Fourth, the excess sugars in fruits and juices turn your body into a petri dish, a perfect breeding ground for opportunistic bacterial infections, while providing little to no usable vitamin C.
For these reasons, supplementation is essential, not because food isn't important, but because it can't deliver what you need and may even become harmful during the flu season.
Vitamin C deficiency weakens resistance to infection, delays recovery, and increases the risk of pneumonia and lung complications. Since vitamin C is rapidly excreted in urine, it's best taken in two doses throughout the day rather than one large amount. I recommend up to 2,000 mg daily during the flu season, divided into two 1,000 mg doses, one in the morning and one in the evening.
Buffered vitamin C in capsules is the best format because (a) it is non-acidic and gentle on the stomach, (b) it provides beneficial, easily digestible calcium, and (c) the capsules dissolve rapidly and are easier to take than tablets.
How to take: Vitamin C is part of the Coenzymated Once Daily Multi formula, but the amount is too low for an immune system boost. I suggest taking this formula alongside the multivitamin: PureWay Vitamin C Capsules.
Vitamin B-complex (B1, B2, B6, B9, B12)
The B-group vitamins act as metabolic catalysts that power nearly every step of energy production, cellular repair, and immune response. They are water-soluble, easily depleted during infection, stress, and fasting, and must be replenished daily through food or supplements.
-
Vitamin B1 (thiamine) supports carbohydrate metabolism and nerve function. Deficiency weakens the heart muscle, lowers stress tolerance, and slows recovery from illness.
-
Vitamin B2 (riboflavin) is required for tissue repair and for the activation of other B vitamins. Low levels lead to mouth sores, skin inflammation, and reduced resistance to infections.
-
Vitamin B6 (pyridoxine) is essential for the formation of immune proteins and antibodies. Its deficiency impairs lymphocyte activity and increases susceptibility to viral and bacterial illness.
-
Vitamin B9 (folate) and B12 (cobalamin) are needed for the production of red and white blood cells. Deficiency causes anemia, fatigue, and reduced oxygen delivery to tissues, all of which compromise immune defenses.
How to take: A balanced B-complex that offers more dependable support than isolated vitamins is included in the Coenzymated Once Daily Multi formula.
The Once Daily Multi formula uses coenzymated, bioactive forms of these vitamins because most people can't properly absorb folic acid, B-12, and B-6, especially if they have the MTHFR gene mutation. Coenzymated vitamins don't need to be converted in the liver or small intestine, so your body can easily absorb and utilize them immediately.
Vitamin B-12 is best taken in sublingual form because it's the quickest way to absorb it. I recommend using this formula: Coenzymated Methyl B-12.
Magnesium
Magnesium is required for more than 300 enzyme reactions that are responsible for energy production, muscle function, and immune response. It regulates the electrical activity of cells, supports normal heart rhythm, and helps control inflammation by stabilizing calcium balance inside tissues.
Low magnesium levels weaken both the nervous and immune systems, increase vulnerability to stress, and promote chronic inflammation that amplifies viral and bacterial damage.
Magnesium deficiency is common due to soil depletion, food processing, and high consumption of refined carbohydrates. Alcohol and medications cause magnesium loss.
The best dietary sources are green leafy vegetables, nuts, seeds, legumes, and magnesium-rich mineral water, but they are best only on paper:
-
Green leafy vegetables are grown commercially in magnesium-depleted soil, so the actual content is far lower than nutrient tables suggest. Cooking or boiling also leaches out a large portion of the mineral into the water.
-
Nuts and seeds contain magnesium, but also high levels of phytates, natural compounds that bind magnesium and prevent its absorption. Roasting or soaking helps only partially.
-
Legumes are high in phytates and lectins that inhibit mineral uptake. People with digestive disorders or low stomach acid absorb even less.
-
Magnesium-rich mineral water varies widely by brand and region, and while it's easily absorbed, the several liters you would need to drink daily to reach an optimal intake isn't practical to consume.
In short, these foods contribute, but they rarely supply enough magnesium for anyone under chronic stress, inflammation, or infection, and even more so for people with digestive problems or who use diuretics, PPIs, or alcohol.
Making things worse, magnesium losses become higher during the infection, while absorption from food becomes poor or absent, and supplementation remains the only viable source.
I prefer magnesium acrobate or citrate formulas because they absorb, assimilate, and act the fastest.
How to take: If you are using the Hydro-CM formula to manage chronic constipation, it already provides all the calcium and magnesium your body needs. Otherwise, I recommend taking this balanced formula: Cal-Mag Caps.
Iron
Iron is essential for oxygen transport, energy production, and immune cell function. It enables red blood cells to carry oxygen to tissues and supports the activity of immune cells that destroy pathogens. Low iron levels weaken both physical and immune strength, leading to fatigue, pale skin, poor concentration, and increased vulnerability to infections.
Iron deficiency is common, particularly in women, older adults, and individuals with chronic inflammation or digestive disorders that impair absorption. However, excessive iron intake can be just as harmful because it stimulates bacterial overgrowth and related side effects.
The best dietary sources of iron are red meat, poultry, and seafood, which contain heme iron that is readily absorbed. Iron from plant sources such as beans, lentils, spinach, and fortified cereals is absorbed far less efficiently, especially in people with low stomach acid. Vitamin C enhances iron absorption, while tea, coffee, calcium, and phytates inhibit it.
The non-heme iron used in fortified foods and inexpensive supplements is a frequent cause of inflammation, bloating, and flatulence. Unlike heme iron from animal sources, non-heme forms (such as ferrous sulfate or ferrous fumarate) are poorly absorbed and highly reactive.
Unabsorbed iron remains in the intestines, where it irritates the mucosa and promotes the growth of pathogenic bacteria that thrive on free iron. This imbalance leads to fermentation, gas formation, and local inflammation, especially in people with preexisting digestive problems or low stomach acidity.
I have a very substantial article on the intricacies of iron deficiencies and supplementation, and recommend reading it to understand better how, when, and why to supplement with iron: How to Self-Diagnose Trace Mineral Deficiencies (Iron).
How to take: Iron is not included in the multivitamin formula because it isn't necessary for people without a deficiency, as explained in the article above. If you need iron, I recommend this formula because it absorbs well and doesn't cause problems common with most iron supplements: Chelated Iron from Ferrochel®
Zinc
Zinc is one of the most critical trace elements for immune defense. It is required for the formation and activation of white blood cells, the repair of mucosal tissues, and the regulation of inflammation. Zinc also helps maintain the integrity of respiratory and intestinal barriers, which block viral and bacterial entry.
Even a mild zinc deficiency weakens immune response, slows wound healing, dulls taste and smell, and increases the duration and severity of respiratory infections. During illness, zinc levels drop rapidly because it is consumed by the immune system and lost through sweat and urine.
The richest sources of zinc are oysters, red meat, poultry, and eggs. Plant sources such as grains, beans, and seeds contain zinc, but phytates and fiber limit absorption.
For supplementation, taking 15–25 mg of zinc daily is sufficient for prevention and immune support. Using higher doses long-term can interfere with copper absorption and should be avoided unless medically necessary.
How to take: Zinc is included in the Coenzymated Once Daily Multi formula.
Copper
Copper works closely with zinc, iron, and vitamin C to support tissue repair, red blood cell formation, and immune defense. It is essential for enzymes that destroy harmful microbes, maintain connective tissue integrity, and regulate inflammation. Copper also helps balance zinc metabolism, while too little copper or too much zinc can disrupt this equilibrium and weaken immune and cardiovascular function.
Cooper deficiency is common, especially in people who take high-dose zinc, consume mostly processed food, or have digestive disorders that impair absorption. Signs of copper deficiency include fatigue, anemia unresponsive to iron, brittle hair, gray hair, and increased vulnerability to infections.
The best dietary sources are liver, shellfish, nuts, seeds, and cocoa. For supplementation, 1–2 mg daily of copper gluconate or bisglycinate is adequate when used alongside zinc in the proper ratio (roughly 10:1 zinc to copper). Long-term intake above 3 mg daily should be avoided because excess copper can accumulate and promote oxidative stress.
How to take: Cooper is included in the Coenzymated Once Daily Multi formula.
Selenium
Selenium is essential for the proper functioning of immune cells and the regulation of inflammation. It supports the enzymes that protect cells from metabolic stress and assists in the production of antibodies and antiviral defense proteins. Adequate selenium levels are associated with lower rates of viral infections, milder disease progression, and faster recovery.
Deficiency impairs immunity, slows recovery, and increases the risk of viral mutation and chronic inflammation. Low selenium intake has been linked to higher rates of influenza, COVID, and other respiratory infections.
The best food sources are Brazil nuts, seafood, eggs, and organ meats. Because the selenium content of plant foods depends entirely on soil concentration, many diets provide insufficient amounts. For supplementation, 100–200 mcg daily of selenium methionine is safe and effective. Intakes above 400 mcg may become toxic and should be avoided.
How to take: Selenium is included in the Coenzymated Once Daily Multi formula.
Iodine
Iodine is best known for its role in thyroid hormone production, but it also has important antimicrobial and immune-regulating properties. The thyroid hormones help produce and control metabolism and energy balance, which in turn determine how efficiently the body mounts and sustains an immune response. Iodine itself has direct antiviral, antibacterial, and antifungal activity on mucosal surfaces, which is why iodine-based antiseptics remain so effective.
Deficiency reduces thyroid hormone output, slows metabolism, and weakens resistance to infection. People with low iodine intake often experience fatigue, feeling cold, sluggish digestion, and increased mucus production — all of which can impair recovery from respiratory infections.
The primary sources are seafood, seaweed, iodized salt, and dairy products. However, many people now use non-iodized gourmet salts or plant-based diets with little or no seafood, leading to gradual depletion. Supplementing with 150 mcg of iodine daily — ideally as potassium iodide or kelp — is sufficient for maintenance. Excessive iodine can overstimulate or suppress the thyroid, so more is not better.
How to take: Iodine is included in the Coenzymated Once Daily Multi formula.
L-Glutamine
L-glutamine is a non-essential amino acid, meaning the body can normally synthesize it, but under stress, illness, or injury, demand often exceeds production. It serves as a major energy source for the cells lining the intestines, immune cells, and other rapidly regenerating tissues.
Glutamine also acts as a nitrogen carrier, helping maintain acid-base balance and support protein synthesis. Because of its dual role in feeding both the gut and the immune system, it becomes a conditionally essential nutrient during infection, inflammation, or recovery, when natural reserves are rapidly depleted.
Supplementation helps restore the integrity of the intestinal lining, reduces inflammation, and supports the recovery of immune cells such as lymphocytes and macrophages. It also improves nitrogen balance and speeds tissue repair after illness or physical stress.
Glutamine is found naturally in meat, fish, eggs, and some dairy products. For supplemental use, 15 to 30 grams daily in powder form is sufficient for maintenance. Higher amounts can be used short-term during recovery from infection, surgery, or intense physical stress.
How to take: I recommend using this formula for the reasons outlined on this page: Glutamine Powder.
Omega-3 Fatty Acids
Omega-3 fatty acids are essential polyunsaturated fats that the body cannot produce on its own. They form part of every cell membrane and help regulate inflammation, immune function, and brain activity. The most active forms, EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), occur naturally in cold-water fish.
The most effective and natural way to obtain omega-3s is from liquid cod liver oil. Unlike capsule-based fish oils, liquid cod liver oil contains a balanced mix of EPA and DHA along with natural vitamins A and D — nutrients that work together to support immune and metabolic health. It is also more bioavailable, easier to absorb, and free from the fillers, gelatin, and oxidation issues often found in capsules.
One teaspoon of high-quality liquid cod liver oil daily provides a sufficient dose of omega-3s for most adults during flu season. The oil should be fresh, refrigerated after opening, and sourced from reputable producers who purify it to remove heavy metals and environmental contaminants.
How to take: My wife and I take this brand that we buy from Amazon: Nature's Answer Cod Liver Oil Liquid Supplement. I am not affiliated with the seller in any way.
Can a Strong Immune System Trigger a Cytokine Storm?
One of the scariest and most deadly complications of COVID-19 is known as a cytokine storm — an uncontrolled immune reaction in which the body releases excessive amounts of inflammatory signaling molecules called cytokines.
In the context of COVID-19, this overreaction occurs when the immune system turns against the body's own tissues. The result is widespread inflammation that damages the lungs, blood vessels, and other organs.
During a cytokine storm, immune cells flood the lungs, causing swelling, fluid buildup, and impaired oxygen exchange. This situation can quickly lead to respiratory failure, blood clotting abnormalities, and multi-organ damage. In severe cases, it's not the virus itself but the body's exaggerated immune response that causes the most serious complications.
Severe outcomes associated with cytokine storms include acute respiratory distress syndrome (ARDS) and multi-organ failure, which together account for the majority of COVID-19 deaths. ARDS alone is responsible for roughly 70% of fatalities linked to cytokine storms.
I bring up this issue because many people assume that when the immune system goes into hyperdrive, it must be "too strong," and therefore it's safer to avoid doing anything to strengthen it.
In fact, the opposite is true. Patients with impaired immunity or lymphocytopenia (low lymphocyte counts) have a higher risk of cytokine storms, ARDS, and poor outcomes.
Cytokine storms occur more often in individuals with weakened immunity due to chronic illness, immunosuppressive treatments, or viral-mediated immune disruption. These conditions prevent proper immune regulation and lead to uncontrolled inflammatory responses.
Chronic diseases such as diabetes, hypertension, cardiovascular disorders, and age-related immune decline predispose people to abnormal cytokine responses. Immunocompromised patients also tend to clear infections more slowly, allowing prolonged immune activation and higher cytokine levels.
As you can see, the cockamamie theory that cytokine storms result from a "strong" immune system comes from the same flawed logic as "if cancer cells use glucose to grow, then eliminating carbohydrates will starve the tumor."
In reality, the body produces glucose even in the absence of carbohydrates by breaking down muscle tissue, and the patient dies of body wasting long before the tumor does. Don't become an easy mark for anyone promoting this nonsense.
Takeaways
The good news is that flu and COVID infections are not inevitable, and your body already has all the systems it needs to prevent them. The following points summarize the key biological, nutritional, and lifestyle strategies that make infection less likely and complications far less severe. They are not complex, costly, or experimental, and grounded in human physiology, not wishful thinking.
-
Preventing infection is possible.In controlled human challenge studies, some volunteers deliberately exposed to COVID-19 never became infected despite receiving identical viral doses. Individual resistance varies widely, proving that infection can be prevented by strengthening metabolic, immune, and digestive defenses.
-
The odds of exposure are high.Each flu season, about one in four (up to 25%) adults contract influenza, and millions more face repeated exposure to COVID-19. Those who maintain strong mucosal barriers and low inflammation often remain uninfected even in shared homes or high-risk settings.
-
Long COVID is more destructive than acute infection.Roughly 17 million U.S. adults report long COVID symptoms such as fatigue, brain fog, and breathlessness that can persist for months or years. Preventing infection altogether is still the most effective protection against this chronic aftermath.
-
Infection and its complications carry real financial and personal costs.Hospital stays average over $3,000 per day, and even short admissions can cost thousands out-of-pocket. Recovery often delays return to work for weeks, causing income loss and reduced productivity. Prevention is far less costly than treatment.
-
Older adults are most affected, but not because of age itself.The highest hospitalization and death rates occur among people over 65, largely because they are in poorer physical shape and take multiple medications that weaken immunity and digestion. Youth is not a reliable defense if health is neglected.
-
Infection outcomes depend on your metabolic state.Viruses thrive in inflamed, nutrient-deficient tissues. Reducing chronic inflammation and restoring metabolic balance make your body less hospitable to infection and improve recovery speed if illness does occur.
-
Insulin drives inflammation and suppresses immunity.Frequent meals, sugary foods, alcohol, sweeteners, and stress elevate insulin. High insulin promotes chronic inflammation, reduces immune responsiveness, and worsens respiratory outcomes. Reducing eating frequency and stabilizing glucose may cut risk by up to 30%.
-
Restoring normal stomach acidity is critical for defense.The stomach's acid barrier destroys pathogens swallowed with saliva or food. Low acidity from dehydration, low-salt diets, PPIs, antacids, or stress allows microbes to reach the intestines. Normalizing acidity may reduce infection risk by another 20–30%.
-
Acid-suppressing and allergy drugs increase vulnerability.PPIs, H2 blockers, and antihistamines disable the stomach's antimicrobial barrier. Long-term users have higher rates of pneumonia and intestinal infections because pathogens survive the stomach and invade the lower tract.
-
Digestive patterns matter as much as food quality.Constant snacking, late meals, and working while eating suppress gastric secretions and slow motility. Unhurried meals at a regular time help improve digestion, maintain normal acidity, and improve food sterilization.
-
Micronutrient sufficiency determines immune capacity.Vitamins A, D, E, C, and the B-complex, together with magnesium, zinc, copper, iron, selenium, and iodine, control every phase of immune response and tissue repair. Even a mild deficiency can blunt immunity or prolong recovery.
-
Animal-based nutrients remain superior to plant substitutes.Red meat, cod liver oil, seafood, eggs, and butter supply bioavailable retinol, heme iron, zinc, and iodine that plant foods cannot match, especially in older adults or those with impaired digestion. These nutrients sustain strong mucosal and immune barriers.
-
Targeted supplementation closes the unavoidable nutritional gap.Even the best diet rarely meets modern micronutrient needs. Coenzymated multivitamins, buffered vitamin C, balanced zinc–copper formulas, magnesium citrate, and moderate vitamin D provide dependable immune support without excess.
-
L-glutamine and omega-3s enhance gut and immune resilience.L-glutamine repairs the intestinal lining and fuels immune cells, while omega-3 fatty acids from liquid cod liver oil reduce inflammation and improve cellular recovery. Together, they strengthen resistance and shorten illness duration.
-
True prevention means creating an internal barrier to infection.Avoiding illness isn't only about masks or distance; it's about biological preparedness. When your metabolism, stomach acidity, and immune defenses function as intended, even high viral exposure may fail to establish infection.
By strengthening the protective mechanisms that nature already built into you, you can stay productive, independent, and free of chronic fatigue or lingering illness, no matter how many seasonal viruses come your way. And even if you do get sick — because no one is immune to bad luck — by following these recommendations, you'll recover faster and walk away intact.
Frequently Asked Questions 
Q. Who else recommends a similar approach?+
I don't know who consolidates all of the above recommendations in one place, but mainstream sources and institutions support my recommendations.
Respiratory health. The Centers for Disease Control and Prevention (CDC) describes respiratory risk reduction as a combination of actions, including masks, distancing, testing, and ventilation, rather than a single solution.
Metabolic health. The National Institutes of Health (NIH) identifies obesity, diabetes, and metabolic syndrome as major risk factors for the severity of SARS-CoV-2 infection. Reviews on insulin resistance describe immune dysfunction links that align with my insulin focus.
Gastric health. The knowledge about the connection between long-term acid suppression and the risk of pneumonia or intestinal infections is a well-established fact in medical literature, and it fully supports my point about maintaining stomach acidity as a primary defense.
Supplementation. The NIH's Office of Dietary Supplements summarizes evidence on vitamins and minerals for COVID-19 positively but warns that supplements are only adjuncts, not primary preventives. I do the same. That's why supplements in my list are in the fourth position, not the first.
I don't know of any individual medical writer or doctor doing comparable work today. The era of celebrity doctors like Robert Atkins, Andrew Weil, Dean Ornish, and Deepak Chopra ended after the market for blockbuster health books collapsed.
Information is now fragmented across social media, podcasts, and niche online publications, leaving no room for a single authoritative voice. I'm sure that if you look hard enough, you'll probably find other people with views similar to mine on Medium or Substack.
And if not, it simply means that I'm a few years ahead of the curve, just as I still am with my work on functional nutrition and digestive disorders.
Q. If COVID-19 vaccines work, why do I still need to follow your recommendations?+
Because viruses mutate, vaccines are not 100% effective, and immunity gradually wanes. Supplements and environmental controls, such as masks, ventilation, and distancing, help reduce transmission, and the CDC still defines prevention as a combination of complementary actions rather than a single intervention.
Your metabolic, mucosal, digestive, and nutritional status add further layers of protection that determine whether exposure remains harmless, causes complications, or becomes fatal.
Q. Do your recommendations replace vaccination?+
No, they do not. Vaccination and natural prevention work on different levels. Vaccines train the immune system to recognize a specific virus, while my recommendations strengthen your body's ability to resist infection in general and recover faster if it occurs.
Relying on vaccination alone, without improving metabolic, immune, and digestive health, still leaves your body vulnerable to complications, long COVID, and opportunistic bacterial infections that vaccines cannot prevent
Q. Why doesn't the government recommend the same approach? +
Governments and public health agencies focus on policies that can be applied to entire populations, not individualized prevention. Nutritional, digestive, and metabolic health depend on personal habits that cannot be standardized or enforced through public policy.
Most official recommendations must be simple to understand, inexpensive to implement, and politically, ethnically, and religiously neutral, which rules out detailed guidance on diet, supplements, or medications.
My approach addresses what those broad guidelines cannot: the specific physiological gaps that determine who gets sick and who doesn't. And it is written for a well-educated audience with the capacity and motivation to act on it.
Q. My doctor disagrees with your recommendations. Why should I listen to you? +
Medical doctors are trained to diagnose and treat disease, not to optimize metabolism, digestion, or nutrition. Most medical education still devotes little time to those subjects, and physicians are required to follow established clinical guidelines, even when those guidelines are outdated or incomplete.
My work focuses on prevention and physiology, not treatment. You don't have to choose between one or the other because your doctor manages your illness, while I explain how to avoid getting one in the first place.
You also need to understand another reality: medical education in the United States emphasizes rote memorization and compliance while discouraging independent analysis or open debate. In a field as complex and high-risk as medicine, that approach ensures uniformity and safety but does not cultivate independent thinking, analytical reasoning, or communication skills.
Q. A friend of mine was a health nut, spent hundreds of dollars on supplements each month, and still died from COVID. Why should I trust you?+
There is a growing class of people, mostly younger, highly educated, and affluent men in the technology field, who fancy themselves "biohackers." They often have sedentary jobs, marginal physical health, and a deep faith that technology can compensate for biology. They treat their health as an engineering project that they can optimize through data, gadgets, and a ton of supplements for every ill.
Because they are relatively young, they can get away with that approach in ordinary circumstances, but there was nothing ordinary about COVID, and that's how many of them got overconfident and dead, unfortunately.
I also spent half of my working life in the technology field, and a similar mechanistic approach to health almost got me killed in my early forties, despite having a fundamental medical education. You can read more about it in my bio: About Konstantin Monastyrsky.
Lucky for me, it happened well before the COVID pandemic, and that's how I became a medical writer. Since then, "less is more" has become my motto and the central thesis of my work. You can learn how well it served me here: Why Should You Trust Me?
Q. Why are infants and toddlers nearly immune to COVID despite their undeveloped immune systems?+
Several physiological advantages protect infants and young children:
Their cells carry fewer ACE2 receptors that the coronavirus uses to infect tissues, which limits viral spread within the body.
Their immune system responds faster and more broadly because it relies heavily on innate immunity, the body's first-line defense..
They have a cleaner diet, don't smoke or drink, have stronger mucus barriers and fewer chronic diseases, and, with a few exceptions, don't take prescription drugs. All of these factors reduce viral penetration and ensuing damage..
In other words, children aren't stronger, but are simply less overwhelmed by problems that compromise most adults. And in many respects, my recommendations regarding metabolic, gastric, and immune health and nutritional status are an effort to bring your body closer to the optimal state of a healthy child.
Q. Isn't inflammation a normal part of the healing process?+
It depends. Acute inflammation is the body's natural repair response to infection or injury, and it resolves once healing is complete.
Chronic inflammation is a different condition entirely. It persists for months or years, even without an active infection, and quietly damages tissues, disrupts immunity, and accelerates aging.
Most modern illnesses — from diabetes and cardiovascular disease to dementia — are the outcomes of chronic, low-grade inflammation.
My goal here isn't to suppress acute inflammation in response to injury, but to prevent it from becoming permanent and from neutralizing your innate and acquired immunity.
Q. Why do you focus so much on high insulin instead of just immunity?+
Because chronically high insulin drives inflammation, suppresses immune function, and disrupts the body's ability to regulate infection and recovery. It also keeps tissues in a constant state of biochemical stress, which weakens mucosal barriers, slows healing, and increases vulnerability to viruses and bacteria.
In practical terms, lowering insulin through natural means does more to restore immunity than any other approach.
Q. I can't afford to purchase the supplements you recommend. What can I do instead?+
Eliminate the foods I don't recommend, eat less food, and eat less often. This way, you'll save more money each month on food than the entire cost of supplements for a year.
Also, the cost is a matter of your priorities. All of the supplements recommended here cost less than $1.50 per day. Missing just one day of work may cost you more than two to three months' worth of supplements. And if you get hit with the flu or COVID, it's never just "one day."
Q. My pastor advocates a clean lifestyle, free of anything factory-made, including supplements.+
A clean lifestyle is always a good foundation, and this article advocates the same approach. Factory-made basic supplements are chemically identical to purified extracts of micronutrients that once came from food, and aren't artificial inventions. They exist because modern food production and storage deplete many essential vitamins and minerals long before they reach your mouth.
The Bible explicitly endorses the use of health-promoting substances to maintain and enhance well-being. The underlying virtue in these references relates to caring for the body as a temple (1 Corinthians 6:19–20).
Q. What if I am already taking supplements from another source?+
That's perfectly fine as long as your supplements are high-quality and made in the United States. Compare what you're taking with the formulations I describe on this site. If the ingredients, amounts, and forms are comparable, there's no reason to switch. The goal is results, not brand loyalty.
Author's Note
Two of the most frequent flu- and COVID-related questions that people ask me are about vaccination in general and my own vaccination status.
Conventional flu vaccines are a statistical gamble. Flu vaccines are formulated months in advance based on predictions of which viral strains might circulate during the coming season. Most years, those predictions miss the mark.
The vaccine may protect you against two or three specific strains, while dozens of others are already spreading. That's why the real-world effectiveness of them hovers between 20% and 50% at best. And that's a speculation as well, because about a similar percent of unvaccinated people don't get infected either.
For these reasons, I haven't taken a flu shot in over 30 years, yet in that time I've had the mild flu only twice despite daily face-to-face work with clients, frequent travel, and an active social life.
In my case, strong digestive, respiratory, and immune health turned out to be far more reliable protection than an annual crapshoot with flu vaccines.
COVID-19 vaccines are a different story. They are not a seasonal guess but the result of precise molecular targeting of the SARS-CoV-2 spike protein — a scientifically validated mechanism that trains the immune system to recognize and neutralize the virus before it can replicate.
Since the beginning of the pandemic, my wife and I have been vaccinated five times with the Pfizer mRNA vaccine. Neither of us experienced any side effects, and the results speak for themselves: no infections, no long COVID, and no health issues afterward.
The flu vaccines don't match the technology behind COVID vaccines because of the biology of the flu virus. It mutates constantly through a process called antigenic drift, meaning that by the time vaccine production ramps up, the dominant circulating strains have already mutated.
If you prefer not to vaccinate for whatever reason from flu or COVID-19 infections, implementing most of the above recommendations will reduce your chance of severe infection, hospitalization, long COVID, and death significantly.
***
If this free article gave you insight into a topic rarely covered by mainstream medical media objectively and in similar depth, that's no accident. I work independently and have no financial ties to pharmaceutical companies, hospitals, or institutional sponsors.
That independence allows me to present the facts without having to serve anyone's agenda. If you find this approach valuable for your well-being, the best way to support my work is by sharing this article with others.
Every repost, forward, or mention helps amplify the reach and makes future work like this possible. Thank you for taking the time to read and for supporting my work!
