How to Restore and Protect Your Energy Metabolism
Age-related energy decline isn’t inevitable. Some people retain normal levels of mental and physical energy well into their fifties, sixties, and beyond. This fact shows that if it is possible for some, it must be possible for all, provided you know how to restore and protect your energy metabolism.
In the previous article, How to Stop Energy Decline at Any Age, I identified and described the top 15 organic factors behind age-related energy decline. They included: (1) Reduced energy metabolism, (2) Reduced structural metabolism, (3) Reduced sleep quality, (4) Reduced digestive efficiency, (5) Weight gain and obesity, (6) Poor dental health, (7) Loss of muscle mass (sarcopenia), (8) Declining bone health, (9) Decreased cardiac output, (10) Loss of vascular elasticity, (11) Glycation, (12) Lower lung capacity, (13) Reduced liver and kidney efficiency, (14) A neurological slowdown, and (15) Autoimmune reactivity.
Some specialists would add the decline of thyroid, adrenal, pancreatic, ovarian, testicular, pituitary, and hypothalamic hormones to this list, but except for some of the ovarian and testicular hormones, that isn't correct. Most hormonal decline isn't caused by aging itself, but by the cumulative effect of the fifteen conditions described above.
No doubt hormone replacement therapy (HRT) for some of these hormones can help to some extent and for some time, but it remains a form of drug treatment that glosses over the underlying causes and carries the risk of side effects, ranging from overstimulation to various cancers.
If you missed that article, I recommend reading it first to give you a clearer understanding of how these organic changes undermine energy from multiple directions.
Seek First to Understand!
I couldn’t write “Energy Metabolism for Dummies” even for a million bucks, because dummies don’t have the capacity to learn, understand, or apply what they’ve learned. And if any of this were simple, the problem of low energy wouldn’t exist in the first place. So let’s begin with the basics.
Energy metabolism is the total set of chemical processes in living cells that generate, store, and use energy to sustain life. It includes the breakdown of molecules to release energy and the building of new molecules or structures that require energy. The key outcome is the continuous production of adenosine triphosphate (ATP) — the universal cellular power source, which drives all other physiological processes.
In other words, cellular energy doesn’t come directly from carbohydrates, proteins, or fats in food or stored in the body’s tissues, but from a chemical molecule (ATP) synthesized inside the cells.
Understanding this distinction is important because low energy can’t be fixed by simply changing your diet to include more or less protein, more or less carbohydrates, or more or less fat. It means that your ENERGY doesn’t depend on the meal composition per se, but on how well your body can convert what you eat into ATP.
That doesn’t mean that you don’t need protein, fat, or carbohydrates — you do, because your organs still rely on them for structure and function, but not for ENERGY. This distinction applies to EVERY SINGLE ORGAN, including the brain. Unlike the popular believe, the brain doesn’t run on glucose or ketones, but on ATP made from them.
If you’re not a biochemist, this distinction may seem trivial — but not to those in the know. Three Nobel Prizes in Chemistry were awarded for ATP-related discoveries as recently as 1957, 1978, and 1997. In science, that’s like yesterday.
— Hey, Konstantin, but what practical implication does all that gibberish mean to me? I am already exhausted just from reading about it.
— Good question, thank you for asking! It means that if you're feeling tired, foggy, sluggish, unmotivated, or just not like you felt in your tens and twenties or thirties, you can’t fix it by switching from avocado toast to fried eggs, or from keto to vegan.
I’m not going to sing the same old song about a healthy diet. Instead, I’m going to give you practical, working guidance on how to increase your energy by fixing its causes and removing the factors that sap it.
To move forward, let’s look at the most common misconceptions about energy and what you can do to eliminate them.
Energy Myths and Misconceptions
Myths and misconceptions lead you to chase hacks, treatments, and shortcuts that don’t exist, ignore the real causes of your energy problems, surrender control of your well-being to false prophets, and keep you from knowing what’s actually right. So, let’s fix that problem first.
Myth #1. Aging causes low energy.
Yes, energy metabolism tends to decline with age, but not for everyone. Here are the numbers from a recent (Feb 2025) study, Prevalence of fatigue and perceived fatigability in older adults: a systematic review and meta-analysis, published in Scientific Reports:
A total of 21 studies involving 17,843 participants were included in this study. The prevalence of fatigue in older adults was 42.6%, and the prevalence of perceived physical fatigability and mental fatigability was 58.2% and 24.0%. [link].
As you can see, the other 57.4%, 41.8%, and 76.0% of older adults do not experience fatigue, physical fatigability, or mental fatigability.
The terms fatigue and fatigability describe the outcomes of low energy metabolism and are functional synonyms of it.
Takeaway: This research goes back to my core thesis: low energy metabolism isn’t universal. With the right know-how or guidance, you can restore much of your energy. It may never be the same at 45 or 55 as it was at 25 — but that isn’t the goal. The goal is to maintain a normal energy metabolism that is appropriate for your age.
Myth #2. Eating turns into energy right away.
No, it doesn't. Your meals may determine how much protein, fat, or carbohydrate your body has available for structure and function, but they don’t determine whether you feel energized or exhausted. That depends entirely on how efficiently your cells can convert those raw materials into ATP — the true fuel of life.
Takeaway: If you feel tired all the time, stop blaming your diet. It’s not about eating more fat, less carbs, or the “right” kind of protein. Your energy doesn’t come from food itself, but from how efficiently your body can convert it into ATP. Until that process is restored, no diet or superfood will make you more energetic. To the contrary, wrong food or excess food will rob you of energy even more.
Myth #3. You can get all the energy you need from a healthy diet.
No, you can't. After all is said and done with regular food, the production of ATP still depends on getting a range of essential micronutrients required for its synthesis.
Theoretically, this is true, but not in practice, and reduced energy metabolism is the very first symptom of their deficiency. If this were otherwise, everyone on a “healthy diet” would be an ageless superman or superwoman.
This section introduces several terms that you may have heard of, but may not be well familiar with their functions. They are:
Mitochondria are small structures inside almost every cell, often described as cellular “power plants” because they convert nutrients into ATP. Each mitochondrion has its own membranes and specialized enzymes that drive the reactions needed to produce ATP.
Substrates. To produce ATP, mitochondria rely on glucose, fatty acids, ketones, and certain amino acids, along with specific vitamins, minerals, and cofactors that support each step of the process. Collectively, they are referred to in medical texts as substrates. When substrates are lacking, ATP production slows, leading to fatigue, weakness, and reduced resilience.
Ketones are energy-rich molecules that are made in the liver from fat during fasting or low-carbohydrate intake. They serve as an alternative substrate for mitochondria, where they are converted into ATP. This contingency allows the body — and especially the brain and muscles — to keep producing energy even when glucose is limited.
The following micronutrients are required for ATP production:
Vitamin B1 (thiamine) is required for helping glucose to reach mitochondria and generate ATP. Instead, the glucose is diverted into the synthesis of lactic acid. The buildup of lactic acid contributes to tiredness, muscle aches, and mental fatigue. Younger adults often get enough thiamine from food to cover this step, but with lower intake in later years, its deficiency becomes more common, and energy levels decline.
Vitamin B2 (riboflavin) is needed to produce coenzymes ( FAD and FMN) that help mitochondria convert fatty acids and glucose into ATP. Without enough riboflavin, fatty acids in particular cannot be fully broken down for energy, forcing the body to rely more heavily on glucose. This deficiency slows overall energy production and leaves people feeling fatigued, especially after exercise, when fatty acids should be the main energy substrate. It also reduces the body’s ability to mobilize body fat for energy — a primary mechanism of weight management (i.e., weight loss).
Vitamin B3 (niacin) is needed to form coenzymes that move electrons inside mitochondria and support the last steps of making ATP. Without enough niacin, this process slows, and the body cannot produce energy efficiently. The result is constant tiredness, poor focus, and low mood, often felt as fatigue that does not improve with rest.
Vitamin B5 (pantothenic acid) is needed to make coenzyme A, which helps carbohydrates, fats, and proteins enter the main energy cycle in mitochondria. Without enough B5, these nutrients can’t be turned into ATP efficiently, and energy production slows down. Low intake often shows up as ongoing fatigue and a reduced ability to cope with stress.
Vitamin B6 (pyridoxine) is required for the enzymes that release glucose from stored glycogen and for converting amino acids into glucose, both of which provide substrates for ATP production. A pyridoxine deficiency limits access to these substrates, leaving the body less able to maintain stable energy metabolism and leading to physical weakness, irritability, and difficulty sustaining recovery and endurance.
Vitamin B7 (biotin) is required for producing enzymes that enable mitochondria to process fatty acids, amino acids, and carbohydrates into substrates required for ATP production. Without sufficient biotin, these substrates can't be utilized. Deficiency reduces energy metabolism, presented as persistent fatigue. Hair loss and brittle nails are two of the most prominent signs of biotin deficiency.
Folate (vitamin B9) is required for developing red blood cells. Folate deficiency leads to anemia, reduces the blood’s oxygen-carrying capacity, and leaves tissues undersupplied with the oxygen needed to produce ATP for normal energy metabolism. This condition often manifests as fatigue, reduced stamina, and difficulty concentrating.
Vitamin B12 is required for developing red blood cells. A lack of B12 leads to anemia, which lowers the blood’s ability to carry oxygen. With less oxygen reaching the tissues, mitochondria cannot produce enough ATP, and energy metabolism slows down. The result is fatigue, weakness, and problems with focus or memory.
Vitamin C is a water-soluble vitamin best known for its role in immunity and structural metabolism, but it is also needed for energy metabolism. It helps the body make carnitine, which carries fatty acids into mitochondria for ATP production, and it keeps iron in a form that can be absorbed and used to deliver oxygen. Without enough vitamin C, both fat conversion into energy and oxygen use decline, slowing ATP output that results in fatigue and slower recovery.
Vitamin A helps regulate the genes that control many enzymes involved in energy metabolism. Without enough vitamin A, the body produces fewer of the proteins needed for mitochondria to make ATP. Low levels often show up as reduced stamina, slower recovery after illness, and a general sense of low vitality.
Vitamin D supports muscle function and mitochondrial activity by helping cells use oxygen more efficiently for ATP production. Deficiency is common with aging and limited sun exposure, and it reduces strength, endurance, and resilience, leaving daily activities feeling harder than they should.
Vitamin E protects the delicate membranes of mitochondria from oxidative damage. Without this protection, ATP production becomes less efficient, and muscle soreness or fatigue appears more quickly.
Vitamin K (especially K2) helps keep blood vessels flexible by directing calcium into bone rather than arteries. When blood flow is restricted, oxygen delivery to tissues declines, limiting the mitochondria’s ability to generate ATP and causing heaviness in the legs and reduced endurance.
Magnesium is required for every molecule of ATP to become biologically active. ATP must bind to magnesium in order to be used by enzymes and cells. Without enough magnesium, the body may still produce ATP, but it cannot use it efficiently. Deficiency often shows up as muscle cramps, restless sleep, and persistent fatigue.
Iron is essential both for hemoglobin, which delivers oxygen to tissues, and for iron–sulfur clusters inside mitochondria, which transfer electrons to generate ATP. Low iron reduces oxygen supply and impairs ATP production, causing exhaustion that does not improve with rest.
Copper is required for synthesizing cytochrome c oxidase (yes, that is how it is spelled), the last enzyme in the electron transport chain. Without copper, the process of making ATP stalls at the final step, leading to weakness and unexplained fatigue.
Phosphorus forms the “P” in ATP (adenosine triphosphate). Without enough phosphorus, ATP cannot be produced in sufficient amounts. Low intake is uncommon in youth but may occur in older adults on restricted diets, causing profound weakness and fatigue.
Sodium, potassium, and chloride maintain the electrical gradients across cell membranes that mitochondria use to pump protons and make ATP. When these electrolytes are low, from diuretics, restrictive diets, or heavy sweating, nerves and muscles cannot function properly, leading to dizziness, weakness, and chronic tiredness.
Iodine is necessary for the synthesis of thyroid hormones that regulate how quickly mitochondria convert nutrients into ATP. Deficiency lowers this “metabolic thermostat,” resulting in cold hands and feet, weight gain, and constant fatigue.
Selenium is required to activate thyroid hormone by converting T4 into T3, the form that stimulates mitochondrial ATP production. Low selenium leaves the body functionally hypothyroid, slowing metabolism and contributing to fatigue and poor resilience.
Manganese is a cofactor for mitochondrial superoxide dismutase, the enzyme that protects ATP-producing machinery from oxidative stress. Inadequate manganese leaves mitochondria more vulnerable to damage, accelerating fatigue and lowering endurance.
L-glutamine is the most abundant amino acid in the body and serves as a backup fuel when glucose is low. It can be converted into the building blocks that mitochondria use to keep producing ATP, especially in muscle and brain tissue. With age, glutamine stores decline, which makes energy output less stable, recovery slower, and periods of stress or illness harder to tolerate.
Carnitine is a compound made from the amino acids lysine and methionine. Its main role is to carry long-chain fatty acids into mitochondria, where they can be converted into ATP. Without enough carnitine, fat cannot be used efficiently for energy, leaving people more dependent on glucose and prone to fatigue and low endurance.
Coenzyme Q10 (CoQ10) is a vitamin-like substance located in the membranes of mitochondria. It transfers electrons along the respiratory chain, a critical step in producing ATP. Levels fall naturally with age and decline further with statin use. Low CoQ10 slows energy output and often leads to weakness, fatigue, and poor exercise tolerance.
Knowing most of this from the biochemistry course I took at medical university, I tried to get all of these nutrients from a healthy diet and even became vegan in 1990, at the age of 46. It didn’t end well, as you can see from the passport photos that didn’t lie:
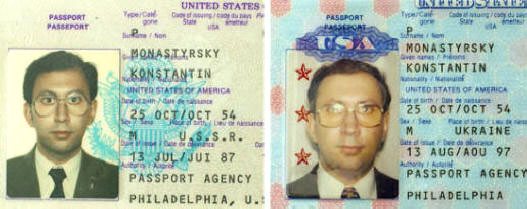
Passport pictures don't lie. Same person ten years apart. From size 34 in 1987 to size 40 in 1997.
By 1994, I was twenty-four pounds overweight, clinically depressed, and suffering from multiple degenerative conditions associated with type 2 diabetes. You can read more about my story in my bio [link].
At 71 (October 2025), I don’t look the same as I did in 1987 or 1997 — but I look better than most men at fifty, let alone sixty. There is only one reason behind this so-called “miracle”: I started taking supplements similar to the ones on this site in 1996, and I haven’t stopped since. That story is described here: Why Should You Trust Me?
Yes, in the opinion of many I “piss expensive urine,” but it’s a small price to pay for being healthy, drug-free, and full of energy at an age when half of my peers struggle to walk a mile, let alone run one.
If you are already taking supplements but they aren’t helping, it usually comes down to three reasons: you’re taking low-quality products, your energy metabolism is being drained by the other 14 factors I described in earlier articles, or both.
Takeaway: The production of ATP depends on adequate substrates — glucose, fatty acids, amino acids, and ketones — as well as the vitamins, minerals, and cofactors that allow mitochondria to process them. When any of these nutrients are lacking, energy output drops sharply at any age.
Ensuring an adequate supply of these nutrients is essential for maintaining stable energy metabolism and normal energy throughout life. For men and women past 40, high-quality supplements are the only viable long-term option to achieve this goal.
Information about the supplements I take myself and recommend to others to restore and maintain peak energy metabolism is available here: Recommended Supplements.
Myth #4. Eat breakfast like a king, lunch like a prince, and dinner like a pauper.
It's the complete opposite. It's best to skip breakfast because it drains more energy than it gives. People expect breakfast to give them energy, but just as often it leaves them sluggish. That’s why you may reach for another cup of coffee by mid-morning, and why the “afternoon slump” often begins hours before noon. Here’s why this happens:
Even light meals divert blood flow and energy resources toward digestion. Heavier meals with protein may stay in the stomach for up to 6 hours before moving on into the intestines. During that time, your body prioritizes digestion over alertness and leaves you tired.
Juices, fruits, sweetened cereals, jam, and coffee or tea with sugar — all cause a rise in blood sugar and insulin, followed by a rebound drop. Low blood sugar is a major cause of your mid-morning fatigue and sugar cravings.
Protein-rich breakfast foods, such as eggs with bacon, divert fluids from the blood into the gut to make digestive juices. This demand, combined with overnight dehydration, can lower alertness until you rehydrate.
While fluids leave your stomach faster than solids, eating and drinking together can still slow the rate at which water and glucose reach your bloodstream, delaying their energizing effects.
Coffee or tea may give you a quick boost, but a few hours later, their stimulant effect fades, which feels even worse if you’re still digesting food or experiencing a sugar dip.
That is why instead of having a stable morning energy and focus, you end up with unstable blood sugar, post-meal fatigue, caffeine fade, and mild dehydration. Doctors and nutritionists even have a term for this condition — postprandial sleepiness, and that is one of the main reasons why I don’t eat breakfast.
Takeaway: By breakfast, I mean the first meal of the day, within an hour after waking up. Move that meal later in the day, ideally toward lunch time. This recommendation doesn’t apply to children, teenagers, and healthy young people under 30, whose physiology is different from people past 40. It also doesn’t apply to people who need to have a meal before taking certain medicines.
Myth #5. You should have a high energy.
Not true! Energy can only be normal or low. It can’t be “high” because it isn’t possible physiologically. A person doesn’t become a world-class marathon runner because they have high energy, but because they are trained to summon the energy they have to complete 26 miles faster than anyone else.
At the end of the run, that person is just as rundown and exhausted as you or I after running a mile, and they take a ton of time to recover before the next run. But they continue to train their bodies and mindsets to use what nature gave them with no more energy than anyone else.
All physiological systems are built with protective brakes to prevent overexertion. When ATP begins to run low, the body triggers fatigue to slow activity before critical systems fail. This self-limiting mechanism applies to muscles, the nervous system, and the brain. What you may perceive as “high energy” in some people is simply normal energy without interference from the roadblocks that diminish yours.
Cells generate ATP at a finite rate. Once the delivery of oxygen, glucose, or ketones falls short or mitochondrial capacity is maxed out, energy production cannot be pushed any higher. The body has no mechanism to exceed this limit, which is why “high energy” doesn’t exist — only normal output or a shortfall when one of these inputs is compromised.
Conditions like bipolar disorder are commonly mistaken for examples of “high energy,” but in reality, they are clinical pathologies. The bursts of activity, sleeplessness, and agitation seen during the hyperactive stage are driven by brain chemistry anomalies, not by greater energy production. These episodes come at the cost of severe crashes, long recovery, and cumulative damage to mood, cognition, and health.
Takeaway: Energy is either normal or low — never above normal. ATP can only be produced at a finite rate, and the body has built-in safeguards that trigger fatigue once those limits are approached. What may appear as “high energy” in yourself or others is more likely a pathology (such as bipolar disorder), a performance, the result of training, or the effect of stimulants — legal or otherwise.
Myth #6. More Protein Equals More Energy.
No, it doesn't. Protein is critical for structural metabolism, but it’s the hardest macronutrient to digest. For many people, especially older adults, heavy protein meals sap energy instead of providing it.
The influencers who promote high-protein diets are false prophets when it comes to restoring energy. Their protein tolerance reflects younger age, years of training, larger muscle mass, and often the use of performance-enhancing substances and stimulants that change how their bodies handle nutrients. None of that applies to the average person. For most people, copying their diets results not in strength or energy, but in bloating, sluggishness, and fatigue.
What you also never see is that they sleep long hours both day and night because of exhaustion, and rely heavily on recovery treatments — ice baths, massages, saunas, stretching routines, hyperbaric therapy, high-dose supplements, and intravenous infusions to restore water and electrolyte balance. Most of them live in favorable climates, with the financial means to support this lifestyle.
Takeaway: Limit high-protein meals to one a day because they take the most time and energy to digest. Do not eat protein bars. They contain the lowest-quality processed plant protein, which is the hardest to digest and keeps your body in a constant state of digestion.
Myth #7. Eating more keeps your energy up.
No, it doesn't. The process of eating and digesting requires a lot of energy. The more you eat, and the more often, the less energy you’ll have left, because so much of it is consumed by digestion, absorption, and assimilation. In other words, the act of “fueling up” can actually drain your energy instead of boosting it. And inversely, eating less often makes you feel more energetic.
This claim is the complete opposite of what you’ve heard all your life from “doctor mom,” “good wife,” health influencers, trendy biohackers, or well-meaning medical professionals repeating what they were taught.
By the time you reach peak growth — usually 18 to 22 for women and 24 to 25 for men — your ability to overeat with impunity is no longer supported by raging hormones, brain development, or structural metabolism focused on growth. At that point, excess nutrients start turning into body fat, reckless behavior, or the misuse of alcohol and drugs to suppress unspent energy.
Takeaway: To normalize energy, start by reducing your meal size and frequency. Drop the breakfast, and avoid constant snacking, grazing, or late-night eating, especially heavy, protein-rich meals.
Give your body time to recover between meals. Eating twice a day within a 6-hour window improves energy within days by reducing the digestive load and freeing up energy resources for focus and movement.
Myth #8. Sugar gives you quick energy.
Not that simple. Sweet foods and drinks may create a brief sense of alertness not because you provided an energy source, but because you triggered the release of insulin, an energy-stimulating hormone. I’ll discuss this topic in great depth shortly.
Naturally sweet foods, added sugars, and artificial sweeteners stimulate the release of insulin in response to sweetness, regardless of actual blood glucose levels. Elevated insulin leads to a rapid lowering of blood glucose. When the body senses this condition, it immediately reduces energy metabolism by turning itself into the energy conservation mode.
Sweetness wasn’t a big part of human nutrition until very recently. All modern fruits have been deliberately cultivated to be much sweeter than their wild counterparts. Even then, fruit was seasonal and available for only a few weeks or months each year. Today’s constant availability of sugar and sweeteners forces the body to handle a metabolic load it was never designed to manage.
Just as with sweetness, insulin was never meant to manage constant sugary foods. Its original role was as part of the fight-or-flight system — mobilizing glucose quickly in critical situations. Once triggered, insulin also sets off other stress and energy hormones. When this system is activated day after day by sweets and sweeteners, it leaves you drained instead of energized.
Over time, constant overstimulation of this system leads to hyperinsulinemia — persistently high insulin levels in the blood. This condition disrupts circulation, damages blood vessels, and fuels chronic inflammation. Both impaired blood flow and ongoing inflammation further drain your energy, leaving you not only tired but also more vulnerable to long-term health problems.
Overexposure to insulin also has a profound impact on character, personality, behavior, mood, sleep, and mental control. When these systems are thrown off balance, the first casualty is energy. Once your mental stability and emotional regulation begin to unravel, your physical energy follows it straight down the drain.
Insulin secretion is also highly conditional. Over years of exposure, your body learns to associate the taste of sweetness with the need to release insulin — even when no actual sugar is present. That is why artificial sweeteners can produce the same effect as sugar itself. Breaking this conditioned response takes time and consistency, but until that adaptation occurs, your energy will continue to drop every time your body anticipates sweetness.
This set of takeaways is very powerful, but it needs a bit of tightening for clarity and flow — while keeping your strong, direct tone. Here’s a polished version with minimal changes, mainly fixing repetition, grammar, and sequencing:
Takeaway: To protect and restore your energy, cut sweetness to zero. Even a hint of sweetness triggers a surge of insulin release, and every surge drains your energy, mood, sleep, and health.
To protect yourself from low blood sugar during the first few weeks, carry sublingual glucose tablets. One tablet — about 3 grams of glucose — is enough to bring your blood sugar back to normal.
Cutting sweetness doesn’t mean cutting out all carbohydrates. Plenty of carbs have no sweetness, and those are fine in moderation. Recognizing this opportunity is especially important for people on diabetes medication, since these drugs add an extra risk of low blood sugar, and they need to consume some carbohydrates.
Once you eliminate all foods with sweetness and keep carbohydrates moderate, type 2 diabetes and prediabetes begin to resolve, blood tests improve, and your doctor will be able to deprescribe your medication. Sugar cravings will disappear, and weight loss will follow naturally.
It is also important to phase out diabetes drugs because many of them work by stimulating insulin release — the very process that keeps draining your energy.
Myth #9. Stimulants give you more energy.
They do, but at a high price. Caffeine, nicotine, and similar stimulants don’t create energy — they only block fatigue signals. This forces you to spend ATP faster, which leaves you even more depleted once the effect wears off. All addiction follows this cycle: stimulant → temporary effect → counter-effect → craving for the next dose.
Energy stimulants such as caffeine, ketamine, amphetamines, and similar agents don’t create energy — they only force your body to spend what it has faster. They work by blocking fatigue signals in the brain or overstimulating neurotransmitters, which makes you feel alert for a time. The cost is that your cells burn through limited ATP reserves more quickly, leaving you more depleted once the effect wears off and increasing long-term strain on your nervous system, sleep, and recovery.
Takeaway: You can fake high energy with stimulants or short bursts of forced intensity, but it isn’t sustainable. The only safe and lasting goal is normal energy. Trying to go beyond “normal” will leave you depleted and eventually broken down. Focus on normal.
Myth #10. Drinking more water boosts energy.
No, it doesn't. Both overhydration and underhydration reduce energy, though by different mechanisms. Too much fluid dilutes electrolytes needed for ATP production, while too little reduces blood volume and oxygen delivery. Either way, fatigue sets in.
Overhydration can reduce energy rather than increase it. Excess fluid dilutes electrolytes such as sodium, potassium, and chloride, which are essential for maintaining the electrical gradients across cell membranes.
These gradients are required for mitochondria to generate ATP. When electrolytes fall below normal levels, ATP production becomes less efficient, leading to weakness, lightheadedness, and fatigue.
Overhydration is not simply a matter of “extra water weight” — it can cause edema, the abnormal accumulation of fluid in tissues. Mild edema may add 5–10 pounds of body mass, while more severe cases can contribute 20 pounds or more. This added mass increases the workload of muscles and joints during routine activity, raising the energetic cost of movement and contributing to fatigue.
Edema also increases the workload of the kidneys, which must filter the excess water and regulate electrolytes under conditions of constant strain. This disrupts fluid–electrolyte balance and interferes with the mitochondria’s ability to generate ATP efficiently.
Another underappreciated effect of edema is the transfer of ambient cold into the body. Excess fluid in the skin and peripheral tissues conducts heat away from the core more effectively, forcing the body to expend more energy maintaining internal temperature. In cooler environments, this thermogenic burden can be substantial, adding yet another pathway to fatigue.
Overhydration can cause a range of side effects, most of which arise from dilution of electrolytes — especially sodium — resulting in hyponatremia. Mild symptoms include nausea, vomiting, headache, bloating, and frequent urination. Moderate to severe cases may include confusion, disorientation, lethargy, muscle weakness, cramping, and swelling of the hands, feet, or lips. In severe instances, overhydration can lead to seizures, coma, respiratory distress (fluid in the lungs), cerebral edema, and, in rare cases, death due to brain and central nervous system dysfunction.
Overhydration can also interfere with digestion. Excess fluid dilutes gastric secretions, slows stomach emptying, and, in susceptible individuals, may contribute to gastroparesis.
Prolonged gastric transit compromises the breakdown and assimilation of nutrients, including the substrates required for ATP production. When fewer substrates reach the mitochondria in a timely manner, energy output declines despite adequate food intake.
Underhydration lowers energy metabolism by a different mechanism. Insufficient fluid decreases blood volume and circulation, reducing the delivery of oxygen and nutrients to tissues.
Since oxygen is required for efficient ATP synthesis, this deficit slows energy metabolism and contributes to tiredness, especially during physical activity or heat exposure. Electrolyte imbalances from dehydration can also cause cardiac arrhythmias, muscle weakness or spasms, and seizures.
Takeaway: Energy depends on balance, not excess. Both too much and too little water interfere with mitochondrial ATP production through different mechanisms. The common advice to “drink more water for energy” overlooks this fact. The real goal is hydration that supports electrolyte balance, oxygen delivery, and normal metabolism, not chasing large fluid intakes.
As you can see, something as trivial as consuming too much or too little fluid can drain your energy significantly, and energy may be the least of your concerns compared to the other complications.
To learn more about this fascinating subject and particularly about how much water to drink, please read the full text of the Water Damage chapter from Fiber Menace. It’s totally free.
Myth #11. More exercise automatically builds energy.
Not right away and not for all. Exercise conditions the body to use energy more efficiently, and moderate physical activity is essential for health. More exercise, however, is not always better for energy metabolism.
In the short term, excessive exercise leads to rapid depletion of muscle glycogen (the stored form of glucose used for ATP production), elevated cortisol and adrenaline levels, and reduced efficiency in using glucose and fatty acids. This produces early onset fatigue, muscle breakdown (catabolism), and impaired recovery.
Excessive perspiration further compounds the effects of overtraining. Sweat carries away sodium, potassium, chloride, and magnesium — electrolytes essential for the electrical gradients that mitochondria require to generate ATP.
Prolonged sweating without adequate replacement causes electrolyte imbalance, muscle weakness, cramps, and less efficient ATP production. Sweating also cools the body, and when exercise takes place under strong air conditioning or in a cool environment, this cooling effect is amplified.
To maintain a safe internal temperature, the body must spend additional energy to reheat the core and vital organs, adding another hidden drain on ATP reserves.
Chronic overtraining disrupts the hormonal systems that regulate energy metabolism, including reductions in thyroid and reproductive hormones, impaired insulin sensitivity, and increased inflammatory markers.
Mitochondrial function may also decline, resulting in decreased ATP production, persistent fatigue, and the condition known as overtraining syndrome. Over time, these disturbances contribute to immune suppression, chronic inflammation, higher risk of illness, mood changes, and loss of lean body mass.
Takeaway: Exercise supports energy only when ATP production can keep pace with demand. Without adequate rest, recovery, and nutritional support, overtraining depletes ATP reserves, disrupts energy metabolism, and leads to chronic fatigue instead of greater vitality. Recognizing early warning signs — persistent tiredness, falling performance, or frequent illness — is essential to prevent long-term damage.
Don’t let it be!
I bet you didn’t expect to get so much actionable information about the factors that reduce energy metabolism. Please use this article as a checklist — not only to understand why fatigue develops, but also to identify which of these factors may apply to you.
As you have seen, energy is not determined by age alone. It depends on the steady production of ATP, which in turn requires balanced hydration, adequate substrates, and the vitamins, minerals, and cofactors that drive mitochondrial function. It is also shaped by lifestyle variables such as diet, exercise, recovery, and stress. When even one of these areas falls out of balance, fatigue becomes inevitable.
Viewed in this context, energy decline and chronic fatigue is not mysterious symptom of “getting older,” but a predictable outcome of specific imbalances. Correcting them may not make you feel twenty again, but it can restore the level of vitality needed to remain fully functional and resilient at any age.
I also want to remind you that low energy is the hidden driver behind a wide range of mental disorders. Depression, anxiety, low motivation, impaired focus, poor memory or dementia-like symptoms, and chronic pain syndromes frequently trace back to energy metabolism that can no longer keep pace with demand. In this light, energy decline and fatigue aren't just about “feeling tired,” but the foundation for many other conditions that damage your health and quality of life. Don’t let it be!
Frequently Asked Questions 
Q. How do I know whether my fatigue is caused by low energy metabolism or by something else, like stress or poor sleep?+
Fatigue from low energy metabolism feels different from ordinary tiredness, especially when it doesn't go away after a good night’s sleep, a weekend of rest, or a change of scenery.
By contrast, fatigue from stress or disrupted sleep tends to fluctuate with circumstances and usually improves after deep rest, a vacation, or a reduction in mental load.
Other signs may include low body temperature, getting cold when others feel fine, brain fog, muscle weakness, caffeine dependence, sugar cravings, chronic migrating pain without an identifiable cause, frequent respiratory infections, irritability, procrastination even with small essential tasks, a persistent feeling of guilt, snapping at others over minor provocations, loss of libido, erectile dysfunction, lack of interest in sex, and loss of appetite.
Many of these patterns are often perceived as depression, a catch-all term for not feeling “normal.” In reality, depression is more likely the expression of a low-energy state rather than the other way around. I believe normalizing energy metabolism should be the first line of treatment for chronic or intermittent depression.
Q. Can energy metabolism be tested directly through blood work or other diagnostic markers?+
There is no single conclusive lab test that can measure “energy metabolism” as a whole because ATP is produced and consumed inside cells within milliseconds, and doesn't circulate in the blood.
What can be measured instead are indirect signs that reflect how efficiently your body is producing and using energy. These measurements include markers of oxygen delivery (such as hemoglobin, hematocrit, and iron studies), thyroid function (TSH, free T4, and T3), blood glucose and insulin levels, electrolyte balance, and basic liver and kidney panels.
Deficiencies in vitamins and minerals that support ATP production, particularly B1, B2, B3, B6, B12, folate, magnesium, and iron, can also be identified through more specialized tests.
The tests can help confirm or rule out major deficiencies, but the final diagnosis always rests on context and observation rather than on a single marker.
Q. If supplements are essential, how soon after starting them should I expect to feel a difference in my energy?+
That depends on how depleted your body is and how long it has been that way. Some people notice subtle improvements within days — clearer thinking, steadier mood, or fewer afternoon slumps — while others need several weeks or even months before their energy normalizes.
Supplements don’t act like drugs or stimulants. Restoring the cellular machinery that makes energy takes time, especially when deficiencies have been long-standing, if digestion and absorption are compromised, or if the immune system is working around the clock to fight off infections and inflammation — a highly energy-demanding process.
Most of the early gains come from restoring the nutrients that directly activate ATP production, particularly B-vitamins, because these have an immediate effect on mitochondrial efficiency.
Keep in mind that B-vitamins are water-soluble and aren’t retained in the body for long, so you need to take them continuously. Their effectiveness also depends on quality — most commercial formulations, including those from top-tier makers, are outdated junk. They look good on paper but do little or nothing once inside the body.
Structural improvements that depend on supplements, such as better muscle tone, mental stability, and recovery capacity, take longer. They involve rebuilding enzyme systems, red blood cells, and tissue integrity — all of which follow slower biological timelines.
The rule of thumb is to give any comprehensive supplementation program at least three to six months before judging results. If nothing changes after that, the problem may not be the supplements themselves but one or more of the other factors that drain energy metabolism, such as overhydration, poor sleep, chronic inflammation, side effects of medications, sugar and coffee addictions, and learned fatigue.
Learned fatigue develops when the body and brain adapt to a chronically low-energy state and begin to treat it as “normal.” You subconsciously avoid effort, movement, or focus because past experiences have taught you that these actions feel exhausting. Even after physical energy is restored, the behavioral pattern of low drive, low expectations, and avoidance remains.
Breaking that cycle requires gradually reconditioning yourself to activity and confidence, not through willpower alone, but by retraining your brain to trust the new reality.
To summarize, supplements can restore what is missing, but they can’t offset uncorrected physiological or emotional causes.
Q. Is it possible to restore energy metabolism without supplements by improving digestion and nutrient absorption alone?+
Improving digestion always helps, but it isn’t enough on its own once energy metabolism has already declined. Better digestion allows you to extract more nutrients from food, but if the food itself lacks those nutrients — or if your body’s demand exceeds what diet alone can supply — absorption won’t solve the underlying shortage. That’s why fatigue and energy decline are common even among people who eat well or take consumer-grade supplements.
Modern diets, even balanced ones, are low in the vitamins and minerals required for ATP production because of soil depletion, food processing, and reduced dietary variety. Add to that the normal decline in stomach acid, digestive enzymes, and intestinal absorption with age, and the gap widens even further.
You can improve digestion through mindful eating, reducing stress during meals, chewing well, optimizing stomach acid, and supplementing digestive enzymes. But that only ensures that available nutrients are absorbed — it doesn’t ensure there are enough of them in the first place.
For adults past forty, supplements are no longer an “add-on,” but a structural necessity. Digestion and nutrient absorption form the foundation of restoration, but supplementation is the glue that holds the structure together. Without it, progress is slow, partial, and easily reversed by even minor illness, stress, or dietary lapse.
This becomes even clearer in adults past sixty. You won’t find a single gerontologist — doctors who specialize in aging — who doubts the role of supplementation, because they see the ravages of nutrient decline far more often than you see them in your own family.
Another issue is maintaining a normal weight. Theoretically, you could eat enough grains, nuts, fruits, and vegetables to get the minimum daily requirements of essential micronutrients, but they come bundled with excess sugars, fats, plant proteins, and water. That combination adds hundreds or even thousands of extra calories to your diet, which will be promptly stored as body fat or, worse, push you toward type 2 diabetes and its countless complications.
That’s exactly what happened to me when, wanting to be “natural,” I switched to a vegan diet at the age of 46, still perfectly healthy and normal weight. Six years later, I was obese and nearly dead from late-stage, undiagnosed type 2 diabetes, which was a commonplace occurrence 30 years ago. If you want to repeat that dumb experience (or experiment), you certainly don’t need supplements.
Q. Can I fast or follow intermittent fasting if I have low energy or blood sugar issues?+
Yes, but not right away and not without preparation. Fasting or time-restricted eating can help restore energy metabolism in the long run, but in the short term, it can worsen fatigue if your system is already depleted.
When energy metabolism is impaired, your cells can’t efficiently switch from glucose to stored fat as fuel. That transition is called metabolic flexibility, and must be rebuilt first by stabilizing nutrient status and restoring normal ATP production.
If you start fasting while your mitochondria are still struggling, your body interprets the fast as starvation, not adaptation. Blood sugar may drop, adrenaline and cortisol surge, and you may experience dizziness, irritability, or brain fog.
Instead of “detoxing,” you end up further exhausting your energy reserves. Once nutritional gaps are corrected and energy metabolism stabilizes, fasting becomes much easier because hunger subsides naturally, energy normalizes, and mental clarity improves rather than declines.
For people with hypoglycemia or diabetes, fasting must be introduced gradually. Begin by spacing meals four to five hours apart, then progress toward a 12- to 14-hour overnight rest from food before experimenting with longer intervals.
Always reduce sweetness first, because every insulin spike during fasting breaks your metabolic rhythm. I discussed this topic in greater depth in the related article.
Proper fasting — intermittent or complete — isn’t about willpower or deprivation; it’s about timing, preparedness, and energy efficiency. Keep in mind that this reply isn’t medical or nutritional advice regarding fasting, but a brief response within the context of a larger discussion on energy metabolism. It’s always best to study the topic further and, ideally, to do so under professional supervision.
Q. Are there early warning signs that my ATP production is starting to slow down?+
Yes, there are, and they often appear years before you begin to feel chronically tired. Most people miss them because they attribute these changes to “aging,” “stress,” or “a busy schedule,” when in fact they are early signs that the body’s energy output is falling below its normal baseline.
The first and most common warning sign is a loss of morning alertness beyond the first hour (which is normal). Long after waking, you continue to feel sluggish or foggy, even after a full night’s sleep.
The second is low basal body temperature — one of the most reliable physical indicators of slowed metabolism. Your basal temperature reflects the amount of heat your body produces at rest, and that heat is generated primarily by ATP. When ATP output drops, body temperature falls with it.
You can measure this at home using a digital thermometer placed under the tongue or in the armpit immediately upon waking, before getting out of bed or drinking water. Record your temperature for several mornings in a row. A consistent reading at least a degree below 97.8°F (36.5°C) suggests your metabolism is running below normal, especially if you also feel cold when others are comfortable, have dry skin, thinning hair, or sluggish digestion.
Please note that consumer-grade digital thermometers are notoriously unreliable and may show readings a degree or more higher or lower than your actual temperature. To check for accuracy, compare your measurement under similar conditions with other family members whose energy and health are considered normal. If your readings are consistently lower than theirs, the difference reflects your state of lower energy metabolism, not a device error.
This state is often followed by declining endurance: climbing stairs, carrying groceries, or concentrating for long periods begins to feel harder than before. Some people also notice cold intolerance because ATP production drives down body heat.
Other early signs include mild anxiety or irritability for no apparent reason, craving stimulants or sweets to “wake up,” slower recovery from exercise or illness, and recurring muscle tension or aches that come and go. You may also see shifts in weight, mood, or appetite that don’t respond to usual efforts. These are the body’s way of signaling that energy metabolism is no longer keeping pace with demand.
By paying attention to these patterns early, you can intervene before fatigue becomes entrenched. Restoring nutrient status, reducing dietary sweetness, improving digestion, and normalizing hydration often reverse these early deficits long before they appear in blood work or medical diagnoses.
Q. Does restoring energy metabolism also help with brain fog, lack of motivation, and bad mood?+
Yes, it does. Your brain consumes about 20% of the body’s energy at rest, so any decline in ATP production shows up there first. When energy metabolism slows, neurons receive less usable energy, and brain function shifts into conservation mode.
The result is what most people describe as brain fog, slower thinking, loss of focus, poor motivation, and procrastination. These changes often precede physical fatigue and are frequently mistaken for depression or burnout.
Once ATP synthesis is restored, the brain’s energy stabilizes. Attention span increases, memory sharpens, and motivation returns because the nervous system is no longer rationing energy.
Mood follows the same pattern: when the brain has enough ATP, neurotransmitter balance improves naturally. You feel calmer, more resilient, and less reactive to stress without needing medication or stimulants.
The brain is hypersensitive to stimulants, both endogenous (from inside the body) and exogenous (external). The endogenous stimulants are stress hormones starting with insulin and escalating through glucagon, cortisol, adrenaline, and noradrenaline, each triggering a stronger but shorter-lived surge of alertness, tension, and eventual energy drain.
Sweetness is an indirect stimulant because it promotes a near-instant release of insulin. That explains why people crave sugar when they’re mentally exhausted. Unfortunately, that fix is short-lived because insulin is a vasoconstricting hormone, meaning it narrows blood vessels and limits oxygen delivery to all organs, including the brain.
Alcohol is also an indirect stimulant because it promotes the release of stress hormones. That’s why some people (mostly men) become hyperaggressive when drunk. For others (mostly women), alcohol has a calming effect because it inhibits glucose metabolism and causes low blood sugar, which, in turn, explains strong sugar cravings when buzzed.
The exogenous stimulants include caffeine, nicotine, MSG, theophylline, theobromine, cocaine, methamphetamine, ecstasy (how appropriate), ephedrine, and prescription drugs such as Ritalin, Adderall, and Dexedrine.
When any of them is withdrawn, the body reacts much like it does to ATP depletion, so you must not confuse true ATP deficiency with withdrawal symptoms.
Interestingly, taking the supplements I recommend may help ease withdrawal and reduce dependence, because many people turn to chemical stimulation as a response to low energy metabolism in the first place.
And not doing it is outright dumb, considering that a 60-day supply of our multivitamin costs about the same as a single bottle of second-rate vodka, scotch, whiskey, bourbon, brandy, or tequila — and doesn’t come with a hangover.
Q. How do medications such as statins, metformin, or thyroid drugs affect energy metabolism?+
Each of these medications interferes with energy metabolism in a different way, although the result is similar: reduced ATP production and persistent fatigue.
Statins (cholesterol-lowering drugs) block the same enzyme pathway in the liver that produces cholesterol and also coenzyme Q10 (CoQ10), which is a critical component of mitochondrial ATP production. When CoQ10 levels drop, mitochondria can’t efficiently transfer electrons to make ATP. That’s why fatigue, muscle weakness, and cognitive dullness are among the most common side effects of statins.
Metformin, widely used for type 2 diabetes, lowers blood glucose by reducing the liver’s glucose output and stimulating insulin release. While that sounds beneficial, metformin also impairs mitochondrial complex I, one of the key steps in ATP synthesis. Many long-term users of metformin develop low vitamin B12 and folate levels, further reducing oxygen utilization and energy output.
Thyroid medications are more complex. In theory, they should improve energy metabolism because thyroid hormones regulate mitochondrial activity. However, when dosed incorrectly—too high or too low—they can either overstimulate or suppress ATP production. Over-replacement may initially increase energy but quickly leads to burnout and muscle wasting, while under-replacement leaves you sluggish and cold because mitochondrial activity remains suboptimal.
All three drugs alter the biochemical reactions behind energy metabolism. It’s essential to counteract their side effects with CoQ10, B-complex vitamins, magnesium, and selenium. Otherwise, the drugs intended to preserve health may quietly damage it.
Q. What happens if I take recommended vitamins and minerals without fixing the other problems you described?+
You may feel some improvement, but not nearly as much as you expect. Supplements can restore what’s missing, but they can’t compensate for habits that keep draining your energy faster than it can be replenished.
Poor sleep, chronic stress, overeating, overhydration, constant snacking, and excessive stimulants all consume ATP at an accelerated rate. As long as those drains remain open, even perfect nutrition can’t restore normal energy metabolism.
In other words, supplements are essential, but lifestyle makes them work. The combination of both is what restores energy metabolism to normal. Doing one without the other is like driving on premium fuel with burned-up spark plugs.
Q. Can women in menopause or men with low testosterone restore normal energy metabolism without hormone therapy?+
The age-related decline in sex hormones that accompanies menopause and andropause — and low energy metabolism — aren’t connected. The first condition in aging men and women is genetically preprogrammed and normal. The second is abnormal.
There is nothing in our genes that says, “When you hit 50, your energy metabolism will go down.” If that were true, young men and women loaded with sex hormones to the gills would never experience fatigue, which obviously isn’t the case.
The misconception about energy metabolism and sex hormones comes from the school of deductive reasoning that goes like this: if sex hormones go down as people get older, and older people don’t have as much energy as younger people, then it must be the hormones’ fault.
Don’t fall for that idiocy. What actually causes age-related fatigue attributed to menopause and andropause are the same things that affect younger people — a slowdown in ATP production caused by all the factors described in the first two articles.
When these factors are corrected and ATP production is restored, many energy-related symptoms blamed on “hormones” diminish or disappear. That happens not because hormones rise dramatically, but because energy metabolism returns to normal.
The other benefits of following my recommendations are that they also halt weight gain, improve appearance, enhance immunity, rekindle libido, restore good mood, prevent aging-related degenerative disease, protect your career, and extend your healthy lifespan.
Q. If I already exercise daily, how can I tell whether I’m helping or harming my energy metabolism?+
The simplest way to tell is by what happens after you exercise. Do you feel clear-headed, calm, and alert within an hour or two? Do you sleep well that night, wake up refreshed, and find your appetite, mood, and focus stable?
If the answers are yes, it means your cells are replenishing ATP as fast as you spend it. But if the opposite is true — you feel high right after a workout but exhausted later, sleep poorly, crave sweets or caffeine the next day, and feel demotivated — those are classic signs that your body and brain are running short on ATP.
What should you do? Study my previous and upcoming articles, and eliminate the factors that drain your energy or suppress energy metabolism. That may also include not exercising daily. Respect your body and your age.
Q. Is it possible to maintain normal energy levels while following a vegan or plant-based diet long term?+
Not really. I’ve already described in several places trying to do the same, and what happened instead. Nonetheless, let me answer again.
Theoretically, a carefully planned vegan diet may supply most essential nutrients, but in practice, it almost never does. Many of the vitamins and minerals critical for ATP production are either absent, poorly absorbed, or present in forms the body can’t efficiently use from plant sources. Over time, these shortages add up and gradually reduce energy metabolism, even with a high calorie intake.
Plant-based diets are also high in natural compounds that bind minerals and further reduce their absorption — fiber, phytates, oxalates, and lectins. The result is the paradox of the “healthy vegan” who eats well yet feels tired, cold, bloated, and mentally foggy. These symptoms reflect a growing deficit in the micronutrients that cells need to produce ATP.
If you choose to remain vegan for ethical or personal reasons, supplementation becomes essential. At minimum, that means high-quality B-complex vitamins, sublingual B12, iron, zinc, iodine, selenium, essential amino acids, and omega-3s from algae to supply the fatty acids missing in plants. Maintaining normal energy metabolism on a plant-based diet without these supplements is virtually impossible, no matter how disciplined you are or how clean your diet may be.
Q. Can ATP supplements restore energy?+
No, they can’t, at least not in the way most people imagine. ATP is an unstable molecule that powers every cell in the body, but it can’t survive digestion or pass intact through cell membranes. In other words, swallowing ATP doesn’t raise cellular energy levels, but only provides raw materials that the body already makes in abundance from food.
The only effective way to “restore ATP” is by improving the process that synthesizes ATP inside your cells. That requires adequate oxygen delivery, a steady supply of glucose and fatty acids, and all of the vitamins and minerals that act as enzymatic cofactors for ATP production. When these factors are restored, your body produces all the ATP it needs.
Q. How do doctors use ATP?+
In clinical settings, adenosine triphosphate (ATP) or its metabolite adenosine is used to:
Interrupt certain abnormal heart rhythms (supraventricular tachycardia). The injected ATP quickly slows the electrical conduction through the heart, restoring normal rhythm within seconds.
Test cardiac function during stress studies, because ATP dilates blood vessels and temporarily increases blood flow.
Relieve severe pain in some cancer patients or during post-surgical recovery, though this use is uncommon.
Research mitochondrial or metabolic disorders, where ATP levels are measured to assess cellular energy production.
Outside these controlled medical settings, ATP isn’t used therapeutically because its effects can’t be replicated through oral supplements.
Q. Can I get enough phosphate from a regular diet, and what are its best sources?+
Yes, almost certainly. Phosphate is the “P” in ATP (adenosine triphosphate). It is also one of the most abundant minerals in the human body, and its dietary deficiency is extremely rare. People easily obtain more phosphorus than they need from a balanced diet, since it’s present in nearly all protein-rich foods.
Phosphorus technically refers to the chemical element, while phosphate is its oxidized form found in the body and in foods. In practice, the two terms are used interchangeably in academic and medical writing, which isn’t strictly correct but is generally acceptable.
The best natural sources of phosphate are meat, poultry, fish, eggs, milk, cheese, and yogurt. Whole grains, legumes, and nuts also contain phosphorus, but much of it is bound to phytates, which makes absorption less efficient. In contrast, animal-based phosphorus is readily absorbed — typically 60% to 80%.
Processed foods, soft drinks, and some fast foods often contain phosphate additives, which are absorbed almost completely. That’s why excess, not deficiency, is the usual concern, particularly for people with kidney disease.
For a healthy person, a varied diet easily provides all the phosphate needed to support ATP production and bone metabolism. There’s no benefit to supplementing it, and doing so can disrupt calcium balance and other electrolytes.
Q. Can some foods reduce ATP production?+
Yes, several common dietary substances can interfere with ATP production, either by blocking the nutrients needed for it or by overloading the system with compounds that hinder mitochondrial function. I already mentioned many of them in the article, but it's worth mentioning the most important culprits again:
Artificial sweeteners and regular sugar. Every spike of insulin triggered by sweetness forces the body into energy-conservation mode once blood sugar falls. Repeated surges blunt mitochondrial efficiency and leave cells less capable of steady ATP production.
Seed oils and trans fats. Highly processed oils (soybean, corn, sunflower, canola) generate oxidative stress inside mitochondria and damage their membranes, lowering their capacity to produce ATP.
Alcohol. Even moderate intake diverts liver metabolism toward detoxifying ethanol rather than making energy. Alcohol also depletes B-vitamins, magnesium, and zinc — all critical for ATP production.
Excessive protein or amino acid supplements. Large, frequent servings deplete ATP for digestion and produce toxic ammonia. The body requires ATP to neutralize ammonia by converting it into urea.
Additives such as MSG, aspartame, and certain preservatives. In sensitive individuals, they can overstimulate neurons and interfere with normal mitochondrial signaling, leading to temporary energy crashes.
Overhydration and electrolyte dilution. Drinking beyond thirst lowers sodium, potassium, and chloride concentrations — the ions mitochondria rely on to generate the electrical gradient that drives ATP synthesis.
Q. Can an ATP deficiency cause death?+
Yes, because life itself depends on a continuous supply of ATP. Every heartbeat, breath, nerve impulse, and muscle contraction relies on ATP as its immediate energy source. If ATP production stops completely, cells lose the ability to maintain their electrical balance and structural integrity within seconds. Irreversible damage follows almost immediately, and death occurs within minutes.
That said, complete ATP failure never happens gradually. It occurs only in catastrophic situations such as cardiac arrest, suffocation, or poisoning that shuts down mitochondrial respiration. In chronic conditions, ATP production simply declines rather than stops, producing fatigue, weakness, poor healing, and eventually organ failure if left unchecked.
Q. Does research support the connection between depression and low ATP?+
Yes, it does. Over the past two decades, a large body of research has linked mitochondrial dysfunction and impaired ATP production to various forms of depression, especially chronic or treatment-resistant types.
The brain is the body’s most energy-demanding organ, consuming about 20 percent of all ATP even at rest. When mitochondrial efficiency declines, neurons are unable to maintain neurotransmitter balance, electrical signaling, and the synthesis of critical molecules like serotonin and dopamine. The result is the common symptoms of depression, such as brain fog, lack of motivation, insomnia, and emotional instability. Micronutrients such as CoQ10, riboflavin (B2), niacin (B3), and carnitine have shown benefit in small clinical trials for people whose depression coincides with reduced energy metabolism.
So while not every case of depression stems from low energy metabolism, the relationship is well established scientifically: when the brain can’t generate enough ATP to sustain its signaling, mood regulation falters. Restoring normal cellular energy often improves not only physical stamina but also emotional balance.
Q. Why did you add MSG to the list of stimulants?+
MSG (monosodium glutamate) isn’t a stimulant in the same sense as caffeine or amphetamines. It doesn’t directly raise heart rate or alertness. I included it because glutamate, the amino acid component of MSG, is the brain’s primary excitatory neurotransmitter. In sensitive individuals, or when glutamate signaling is excessive, it can overstimulate certain neurons — a process called excitotoxicity. That overstimulation temporarily increases neural firing and metabolic demand, which consumes ATP more rapidly and can lead to an energy “crash” afterward.
For most people, moderate MSG intake is metabolically neutral. But in people who already have impaired energy metabolism or low magnesium status, even small surges in glutamate activity can tip the balance toward fatigue, irritability, or headache — symptoms that mimic overstimulation. So MSG isn’t classified pharmacologically as a stimulant, but it can act as an excitatory agent under certain physiological conditions, which is why I grouped it with substances that transiently drive energy use upward before causing depletion.
Q. Why are some overweight or obese people full of energy?+
Because excess body weight doesn’t automatically mean low energy metabolism, many overweight and obese individuals still have strong mitochondrial capacity and an efficient supply of oxygen, nutrients, and hormones to their tissues. What drives energy levels isn’t the amount of fat stored, but how well that fat — along with glucose and amino acids — can be converted into ATP inside cells.
People who stay energetic despite carrying extra weight often share several traits:
Stable blood sugar control — they may eat regularly, avoid sharp glucose swings, and maintain adequate B-vitamin and magnesium levels that support ATP synthesis.
Good cardiovascular conditioning — even modest activity, such as walking or light physical work, keeps circulation and oxygen delivery strong.
Adequate micronutrient intake — diets high in calories sometimes still provide enough cofactors for energy metabolism.
Resilient nervous systems — low chronic stress and sufficient sleep allow the body to recover and maintain hormonal balance.
In contrast, people with the same or lower body weight but sluggish energy usually have one or more of those systems compromised — nutrient deficits, poor oxygen delivery, or high insulin and cortisol that blunt mitochondrial output. Fat storage and energy production are related but distinct processes; it’s entirely possible to be energetically efficient but metabolically imbalanced, which is why some obese individuals feel vigorous while thinner people can feel constantly drained.
Q. Is there a medical specialty or doctors who specialize in energy restoration?+
Not really. No medical specialty focuses specifically on restoring energy metabolism. Conventional medicine treats fatigue as a symptom rather than a condition, so doctors usually look for an underlying disease such as anemia, thyroid imbalance, diabetes, heart failure, or depression.
If none is found, the patient is often told that everything is “normal,” or it’s in their heads (you’re weak-minded), it’s psychosomatic (you’re crazy), it’s idiopathic (cause unknown), and similar other garbage instead of the honest “Sorry, I don’t know.”
Q. Can you help me restore energy?+
Yes. That is exactly what my work is about. I consult one-on-one to evaluate diet, supplements, sleep, hydration, medications, and other variables that determine how efficiently your body produces ATP.
There is no single magic advice or fix. Restoring energy is a process. Many factors are involved, and they must be unwrapped one by one in a clear sequence. We start with the most impactful causes, stabilize them, then address the remaining ones. Some people notice changes in days, but durable normalization usually takes weeks to months.
If you want personal assistance, you can schedule a brief introductory call to review your situation and outline a step-by-step plan. The goal is not to “boost” energy temporarily, but to restore normal energy metabolism steadily and permanently.
* * * *
If you still have a question that isn’t covered here, please email it to me. If it’s broad enough to be relevant to others, I’ll add it to this list in the next update. And if you need personal assistance with resolving your own energy issues, I work with clients one-on-one by consultation.
Author’s Note
Age-related energy decline is the primary reason behind career failures across an entire working life. The decisive factor in long-term success is not intelligence, appearance, social skills, or the connections that open doors at the start, but solid character supported by sustained energy.
Investment banks, law firms, ad agencies, consulting companies, and venture capital firms know this well. They weed out low-energy individuals among equally talented recruits during the first two to three years of demanding work. Those who survive advance toward partnership, while those who can no longer sustain the pace are quietly let go.
Share this material with your adult children, siblings, colleagues, and friends who may be affected by low energy. If you run a business, share it with your employees. Improving the energy and health of your staff by just 20 to 40% is equivalent to adding two to four more people to your team without the cost of recruitment, salaries, benefits, or onboarding.
***
If this free article gave you insight into a topic rarely covered by mainstream medical media objectively and in similar depth, that's no accident. I work independently and have no financial ties to pharmaceutical companies, hospitals, or institutional sponsors.
That independence allows me to present the facts without having to serve anyone's agenda. If you find this approach valuable for your well-being, the best way to support my work is by sharing this article with others.
Every repost, forward, or mention helps amplify the reach and makes future work like this possible. Thank you for taking the time to read and for supporting my work!
