What exactly are normal stools?
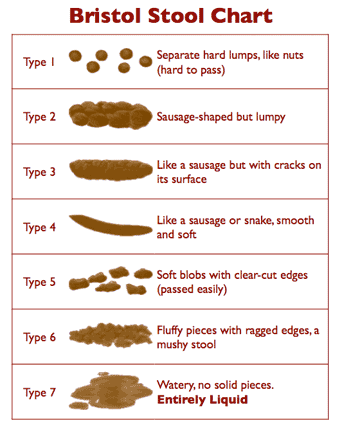
Researchers at the Bristol Royal Infirmary—a hospital in Bristol, England—developed a visual guide for stools. It is called the Bristol Stool Form Scale, or BSF scale for short. It helps skittish patients and doctors to distinguish normal stools from abnormal without getting embarrassed over personal details.
The normality of ones' stools is determined by comparing them to the Bristol Stool Form scale, or the BSF scale for short. The 'Bristol' in the BSF refers to the Bristol Royal Infirmary — a hospital in Bristol, England -- from where this scale originated.
It is a self-diagnostic chart designed to help skittish patients discuss this delicate subject with their doctors without getting embarrassed. This is, essentially, what the Brits call getting the “royal treatment…”
You just look at a simple chart, point to what approximates the content of your toilet bowl, and your doctor (or this page) tells you whether the form is right or wrong.
» Type 1: Separate hard lumps, like nuts
Typical for acute dysbacteriosis. These stools lack a normal amorphous quality, because bacteria are missing and there is nothing to retain water. The lumps are hard and abrasive, the typical diameter ranges from 1 to 2 cm (0.4–0.8”), and they‘re painful to pass, because the lumps are hard and scratchy. There is a high likelihood of anorectal bleeding from mechanical laceration of the anal canal. Typical for post-antibiotic treatments and for people attempting fiber-free (low-carb) diets. Flatulence isn‘t likely, because fermentation of fiber isn‘t taking place.
» Type 2: Sausage-like but lumpy
Represents a combination of Type 1 stools impacted into a single mass and lumped together by fiber components and some bacteria. Typical for organic constipation. The diameter is 3 to 4 cm (1.2–1.6”). This type is the most destructive by far because its size is near or exceeds the maximum opening of the anal canal‘s aperture (3.5 cm). It‘s bound to cause extreme straining during elimination, and most likely to cause anal canal laceration, hemorrhoidal prolapse, or diverticulosis. To attain this form, the stools must be in the colon for at least several weeks instead of the normal 72 hours. Anorectal pain, hemorrhoidal disease, anal fissures, withholding or delaying of defecation, and a history of chronic constipation are the most likely causes. Minor flatulence is probable. A person experiencing these stools is most likely to suffer from irritable bowel syndrome because of continuous pressure of large stools on the intestinal walls. The possibility of obstruction of the small intestine is high, because the large intestine is filled to capacity with stools. Adding supplemental fiber to expel these stools is dangerous, because the expanded fiber has no place to go, and may cause hernia, obstruction, or perforation of the small and large intestine alike.
» Type 3: Like a sausage but with cracks in the surface
This form has all of the characteristics of Type 2 stools, but the transit time is faster, between one and two weeks. Typical for latent constipation. The diameter is 2 to 3.5 cm (0.8–1.4”). Irritable bowel syndrome is likely. Flatulence is minor, because of dysbacteriosis. The fact that it hasn‘t become as enlarged as Type 2 suggests that the defecations are regular. Straining is required. All of the adverse effects typical for Type 2 stools are likely for type 3, especially the rapid deterioration of hemorrhoidal disease.
» Type 4: Like a sausage or snake, smooth and soft
This form is normal for someone defecating once daily. The diameter is 1 to 2 cm (0.4–0.8”). The larger diameter suggests a longer transit time or a large amount of dietary fiber in the diet.
» Type 5: Soft blobs with clear-cut edges
I consider this form ideal. It is typical for a person who has stools twice or three times daily, after major meals. The diameter is 1 to 1.5 cm (0.4–0.6”).
» Type 6: Fluffy pieces with ragged edges, a mushy stool
This form is close to the margins of comfort in several respects. First, it may be difficult to control the urge, especially when you don‘t have immediate access to a bathroom. Second, it is a rather messy affair to manage with toilet paper alone, unless you have access to a flexible shower or bidet. Otherwise, I consider it borderline normal. These kind of stools may suggest a slightly hyperactive colon (fast motility), excess dietary potassium, or sudden dehydration or spike in blood pressure related to stress (both cause the rapid release of water and potassium from blood plasma into the intestinal cavity). It can also indicate a hypersensitive personality prone to stress, too many spices, drinking water with a high mineral content, or the use of osmotic (mineral salts) laxatives.
» Type 7: Watery, no solid pieces
This, of course, is diarrhea, a subject outside the scope of this chapter with just one important and notable exception—so-called paradoxical diarrhea. It‘s typical for people (especially young children and infirm or convalescing adults) affected by fecal impaction—a condition that follows or accompanies type 1 stools. During paradoxical diarrhea the liquid contents of the small intestine (up to 1.5–2 liters/quarts daily) have no place to go but down, because the large intestine is stuffed with impacted stools throughout its entire length. Some water gets absorbed, the rest accumulates in the rectum. The reason this type of diarrhea is called paradoxical is not because its nature isn‘t known or understood, but because being severely constipated and experiencing diarrhea all at once, is, indeed, a paradoxical situation. Unfortunately, it‘s all too common.
Interestingly, the interpretations and explanations of the BSF scale that accompany the original chart differ from my analysis. To this I can only say: thanks for great pictures, but, no thanks for the rest...
Excerpted from Fiber
Menace, page 117-120;
BSF Chart: wikipedia.org
To avoid referencing non-descriptive numbers, I use the following definitions: types 1, 2 and 3 = hard or impacted stools. Type 4 and 5 = normal or optimal. Type 6 = loose stool, subnormal, or suboptimal, and type 7 = diarrhea.
In such cases as acute hemorrhoidal disease, anal fissure, or the inability to attain unassisted stools, loose stools (type 6) are acceptable. It‘s a messy experience, but which would you rather have — a bucketful of blood, pain, and a wound that won‘t heal, or a little lukewarm douche afterwards?
To restore and maintain normal stools (from type 4 to 6), the colon and rectum must first be free from hard stools (from type 1 to 3). In our case, the opposite of “hard” isn‘t “soft,” but difficult (not easy) or irregular.
As you can see from the illustration (and, perhaps, already know firsthand) “hard” stools can be “small,” “regular,” and “large.” Equally important, a “small” stool for one person can be “large” for another, because the perception of size isn‘t determined by a caliper, but by the aperture of one‘s anal canal. If the anal canal is constrained by enlarged internal hemorrhoids, even “small” stools, such as type 4, may be “difficult” to pass. Don‘t fall into this trap. The rule is: If stools are hard as in difficult, or not easy, or irregular, they are HARD, period!
Unless your stools are type 4 to 6 (normal), they are impacted. Impacted stools can be small, large, hard, soft, dry, moist—it doesn‘t matter. What “impacted” means is that they had a chance to pile up and compress in the large intestine. Despite all of the nonsense you‘ve been hearing about “formed” stools, if yours are “formed,” they are impacted.
If we didn‘t have the Bristol Stool Form scale illustration in front of us, and you asked me what are normal stools, I would answer: normal stools are not noticeable during defecation!
Again, for someone with an intact anal canal, this may consist of formed stools as in type 4. For someone with hemorrhoidal disease, this may only be loose stools as in type 5 or 6. In other words, the normality differs from person to person, depending on the degree of prior damage. It‘s pretty much similar to defining pornography in the context of free speech: I can‘t tell you what pornography is, but I can tell when I see it. Similarly, I can‘t tell you what normal stools are, but you can tell when you don‘t have them.
As you can see from the BSF scale, normal stools don‘t have to be round. After all, your anal canal isn‘t really round (when shut, it‘s actually flat), particularly if you already have enlarged internal hemorrhoids. So a flat shape is okay. In fact, when stools are already round as in type 4, it means you already have a slight degree of impaction. Otherwise their shape would be flattened up while passing through the anal canal.
Flat stools scare doctors a great deal because type 2, 3 and, to a lesser extent, type 4 may indicate the presence of a colorectal tumor. But that's because few doctors have ever observed normal (type 5) stools themselves.
Here is what's actually happening: think of the colon as a round mold. Then, it‘s easy to imagine why a tumor may change impacted stools from the round shape to a flat shape. This rare occurrence doesn‘t apply to type 5 stools, because their shape is formed primarily by the shape of the anal canal, not the colon‘s “mold.”
To rule out a tumor scare — don‘t panic! Withhold your stools for few days to give them the opportunity to get molded. Observe their shape, and calm yourself down and your doctor.
Let's summarize:
- Abnormal stools are any stools that require straining and/or you feel pressure from stools passing through the anal canal.
- Abnormal stools may be small or large size-wise, depending on fiber consumption, and frequency of defecation.
- Normal stools can be loose or slightly formed (Such as BSF type 5).
- Normal stools (between BSF type 4 and 6) aren‘t perfectly round.
- Normal stools for one person may be abnormal for another. The degree of normality is determined by the anatomy of the anal canal.
- Normal stools require zero effort and zero straining for elimination.
- Normal stools pass through the anal canal without any perception of pressure.
Of course, once you have damage to the anal canal, achieving absolute “normality” may be hard. So you may have to accept a small degree of “abnormality” such as type 6 stools. This is no different from accepting gray hair, wrinkles, dental implants, and so on.
You may also have to live with the fact that after a certain degree of prior damage, caused by fiber, you won‘t be able to attain “unassisted” defecation and “normal” stools because of irreversible nerve damage, stretching of the large intestine, significantly enlarged hemorrhoids, and similar factors. I‘ll teach you how to overcome this problem as well without fiber and laxatives.
In fact, if I didn‘t know how to attain this seemingly impossible goal, I wouldn‘t be touching this subject or this site. I only got into this game when I was assured of a winning hand.
Reader's testimonial “Although I have been using your products for only
two days, I can say with no hesitation that your
products work. I am amazed they are working so
quickly.
Thank you again for creating a truly wonderful
product. I hope that you are able to spread the
truth far and wide and that hundreds of thousands of
people achieve better health because of your
outstanding work. One person truly can make a
difference.” L.C., USA (via e-mail)
A generation or so ago the term “costivity” was broadly used to describe hard stools and straining, while the term “constipation” was used to describe “irregularity,” meaning “a failure to move the bowels daily.”
Since then, the terms costivity and constipation have blended into one, while the “failure to move the bowels for three consecutive days” has become the 'official' definition of clinical constipation.
On the other hand, painful and bloody stools within these three days has become a mere irregularity, or a doctor-speak for “don't bore me with your problems until the fourth day.”
In practical terms, this means that the definition of “constipation” has become too vague and unspecific — a situation akin to doctors not knowing the location of your heart or liver. Indeed, how can you get proper treatment, when constipation for you means “pain while moving the bowels,”, while it may mean the “failure to move the bowels for three consecutive days” for your doctor!
For this and other practical reasons I reclassified constipation (see Fiber Menace, p.p. 97-128 for more details) into three distinct stages: functional (reversible), latent (hidden), and organic (irreversible):
- Functional constipation. This condition commonly follows a stressful event, surgery, colonoscopy, diarrhea, temporary incapacity, food poisoning, treatment with antibiotics, the side effects of new medication — the circumstances that damage intestinal flora, interfere with intestinal peristalsis, or both. A person becomes irregular, stools correspond to the BSF scale type 1 to 3, and straining is required to move the bowels. The person resorts to fiber or laxatives for help.
- Latent constipation. If the intestinal flora, stools, and peristalsis aren't properly restored following adverse event(s), functional constipation eventually turns into the latent form (i.e. hidden), because fiber‘s or the laxative's effects on stools create the impression of normality and regularity. The stools become larger, heavier, and harder, usually the BSF type 3, straining more intense, but for as long as you keep moving your bowels every so often, and without too much pain, there is still an impression of regularity. This is, by far, the most dangerous form of constipation because of what happens next...
- Organic constipation. As time goes by, large and hard stools — between type 2 and 3 — keep enlarging internal hemorrhoids and stretching out the colon. This, in turn, reduces the diameter of the anal canal even more, causes near complete anorectal nerve damage, and slows down or cancels out completely the propulsion of stools alongside the colon (motility). At this juncture, the person no longer senses a defecation urge, and becomes dependent on intense straining and/or laxatives to complete a bowel movement. If you don't use 'hard' laxatives, you fail to move the bowels even with a good helping of fiber. That is, in fact, what most people mean nowadays when they say: “I have been diagnosed with constipation.”
So, as you can see, you can indeed use fiber to coax your bowels into regularity for a good while, but at the expense of enlarged stools. At some point in that 'while,' you'll also end up with damaged bowels, and a life-long dependence on more and more fiber, and 'hard' laxatives
How long that 'while' may last depends on how early you get started with this crazy therapy. If you are in your teens today, you'll pay the price in your early forties, if you are in your early forties, damnation will come by your early fifties. If you are a woman, things will go downhill even faster for reasons explained on this page: Why Women Get Constipated More Often Than Men?
How to overcome constipation by “normalizing” stools
Constipation rarely happens out of the blue in otherwise healthy adults. It is usually preceded by decades of semi-regular stools that are either too large, or too hard, or both. These abnormal stools cause gradual nerve damage and enlargement of the colon, rectum, and hemorrhoidal pads until one day the bowels refuse to move as was meant by nature — once or twice daily, usually after a meal, and with zero effort or notice. Therefore, it's best to recognize and eliminate abnormal stools long before they bite you in the butt, literally and figuratively.
To attain small stools and effortless bowel movements immediately— use the Hydro-CM program. The duration depends on the degree of acquired colorectal damage. The goal is to eliminate straining, reduce pressure on internal hemorrhoids, and restore anorectal sensitivity.
For a comprehensive, life-long recovery, start from this section: No Downside, Just Upside-down.
You may also find relief by reviewing the answers to the following questions:
Q. Why do women get constipated more often than men?
Q. What is the difference between irregularity and constipation?
Q. Is constipation dangerous for my health?
Q. How often should I move my bowels?
Q. Why do some foods cause constipation?
Q. Does stress cause constipation and why?
Q. Does alcohol cause constipation?
Q. Why does anal sex cause constipation?
Q. What causes traveler's constipation?
Q. Why is my infant constipated?
Q. Why is my toddler suddenly constipated?
Q. What are the causes of constipation in older children?
Q. What is the connection between autism, infant constipation and diarrhea?
Q. What is the connection between constipation and the epidemic of juvenile diabetes?
Q. Why do doctors recommend fiber to treat constipation?
Q. Is it true that dietary fiber prevents or relieves constipation?
Q. Can I relieve constipation by drinking more water?
Q. Is it true that regular exercise stimulates intestinal activity?
Q. Is it true that toning up lax muscles helps to relieve constipation?
Q. Is it true that animal fat causes constipation?
Q. Why do Atkins-style diets (i.e. low-carbohydrate) cause constipation?
Q. What is the best diet for constipation relief?
Q. Why do antibiotics cause constipation?
Q. Does smoking cause constipation?
Q. Why does colonoscopy cause constipation?
Q. Why does surgery cause constipation?
Q. Why does hot weather cause constipation?
Q. Can constipation cause acne?
Q. What are the causes of constipation during pregnancy?
Q. Why does constipation cause enlarged internal hemorrhoids?
Q. Why does constipation cause anal bleeding?
Q. Why does constipation cause bloating and flatulence?
Q. Why does constipation cause chronic fatigue?
Q. Can constipation reduce my immunity?
Q. Can constipation cause bad mouth odor?
Q. Is it true that old stools can cause “encrustation” of the large intestine‘s walls?
Q. What is the connection between constipation and appendicitis?
Q. What is the connection between constipation and colorectal cancer?
Q. What are the most common side-effects of traditional laxatives?
Of course, you may opt to do nothing, continue to strain and use fiber and/or laxatives, and we'll meet again several years from now, except the next time around it will be even more difficult, involved, and expensive to return to normality. That's, unfortunately, the nature of the beast — as the years pass, colorectal disorders related to abnormal stools become more severe, and the damage— irreversible!
Also, if you are a parent or a guardian of a young child, use this chart to fix minor problems well before they become a major headache for you and a source of life-long trouble for your child.
Strange, but true — the content of your toilet bowl predicts your future with more certainty than a crystal ball. With that in mind, read up, look down, and stay well!