Hemorrhoids and anal fissures: What nature giveth, Newton's Law taketh away
Hemorrhoidal disease and anal fissures start with a little "defect" in human anatomy — the anal canal that is too darn tight for large and/or hard stools to pass through. When these abnormal stools get stuck inside the colon or rectum, you may have no choice but to strain, and gradually causing yourself hemorrhoidal disease, anal fissures, and other complications.
All things considered, early stage hemorrhoidal disease is the least bothersome outcome of straining — it isn't unheard of individuals to pass out from severe pain, getting heart attack, or dying from stroke while moving bowels. Despite these considerable risks and lethal outcomes, straining isn't only considered normal, but is also encouraged by doctors who advise patients to strengthen their abdominal and pelvic muscles, so they can strain even harder.
By the time the damage from straining become apparent through pain, prolapsed hemorrhoids, bleeding anal fissures, purulent fistulas, rectocele (the prolapse of the rectum wall into the vagina), megacolon, or diverticular disease, the stools are getting even larger and harder because of incomplete emptying of the bowels. This condition results from involuntary contraction of the anus and the termination of the intestinal peristalsis in response to pain (and fear) related to all of the above complications.
Some people, especially children, intentionally withdraw stools to avoid pain. This habit may lead to fecal impaction — a formation of a large lump of solidified feces (fecaloma) inside the rectum or the colon. Fecal impaction in the rectum requires manual —with a finger — disimpaction, a procedure that has the potential to cause even more emotional and physical trauma, particularly for a child. Fecal impaction inside the colon may require emergency surgery to resolve it [link].
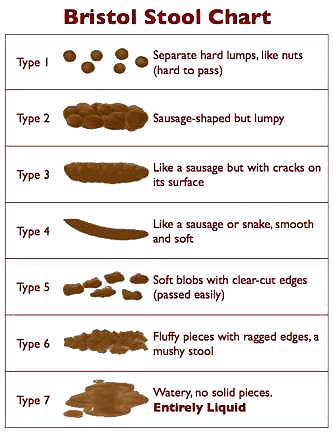
Large stools — as in the Type 2 and 3 in the Bristol Stool Chart below — aren't defined by their volume, but size, or, to be exact, their diameter. The stools turn "large" for the following reasons:
 Source: Wikipedia; licensed under the Creative Commons [link]
Source: Wikipedia; licensed under the Creative Commons [link] - A diet high in processed fiber. Dietary fiber is the only known substance capable of enlarging your stools.
- Taking synthetic or fiber-based bulking laxatives. This is why indigestible fiber in foods and laxatives is universally referred to by doctors as a "bulking agent."
- Chronic constipation. While defined by Western doctors as inability to move bowels in three consecutive days, it is flat out wrong. A proper definition is not moving bowels at least once daily, needing to strain, needing to take fiber laxatives or consuming laxogenic foods such as beets, prunes, prune juice, flaxseeds, and fiber-fortified cereals, bread, and pasta, or all of the above.
- Conscious withdrawal of stools due to pain or circumstances, such as lack of clean bathroom, no access to bathroom facilities when needed, concerns over privacy, and other similar concerns.
- A diet low in sodium chloride (table salt), excessive sweating or acute dehydration. These conditions cause a rapid extraction of sodium chloride and fluids from feces.
- The use of common medications and illicit drugs that affect the function of smooth muscles, and diminish intestinal peristalsis (antidepressants, antihypertensive, anticonvulsants, opioids and others [link].
- A diet low in dietary fat because fat is a primary factor that commands the body to initiate gastrocolic reflex and peristaltic mass movement.
- Endocrine disorders such as underactive thyroid or adrenal insufficiency. These conditions adversely affect the function of smooth muscles of the colon and rectum.
- Diabetes-related anorectal nerve damage. This condition reduces the sensation of urge, so the person doesn't feel a need to defecate.
- Incomplete bowel emptying regardless of causes most often related to pain and preceding complications.
You may have heard that stools may get hard and dry from dehydration, but that isn't true. Stools may turn as hard as rock when their moisture content drops as little as 10% to 20% — a mere drop inside the "sea of water" that the human body actually is. I discuss this paradox at length here: Is it true that drinking more water prevents or relieves constipation?
I wish everything connected to the mere act of forming stools and moving bowels wasn't so complicated, but it is, and here is why...
The final frontier between you and the toilet bowl
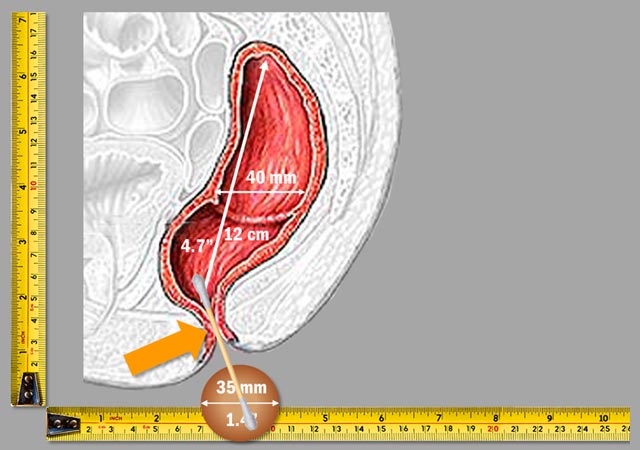
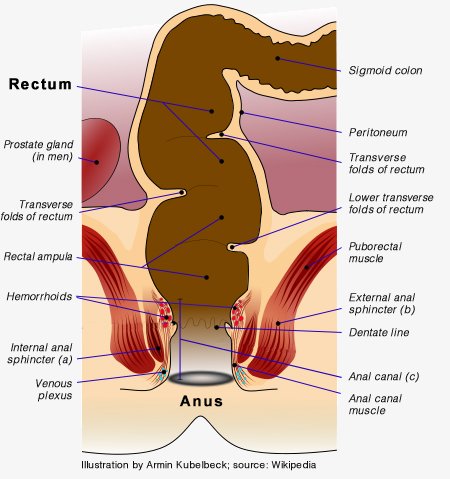 The anus ("ring" or "circle" in Latin) is made from the two circular bands of muscle that encircle the exit of the rectum. The inner band — the internal anal sphincter (a) — is involuntary. The outer band — the external anal sphincter (b) — is voluntary.
The anus ("ring" or "circle" in Latin) is made from the two circular bands of muscle that encircle the exit of the rectum. The inner band — the internal anal sphincter (a) — is involuntary. The outer band — the external anal sphincter (b) — is voluntary.
Working in concert, both sphincters relax and open in order to allow feces and/or gases to exit the rectum. The term "anal canal (c)" refers to the passageway formed by the opening of both sphincters, usually during bowel movement.
At any moment, you can make a conscious decision to tense the external anal sphincter (b) and terminate the bowel movement or retain flatus. The ability to keep feces and flatus inside until you consciously decide to move bowels or release gases is an essential social skill acquired by around the 3rd birthday. If not for this mind over fecal matter faculty, there would be no civilized society as we know it.
Our voluntary ability to control the external anal sphincter isn't limitless. When the intra-rectal pressure becomes too strong, such as during diarrhea or when there is large volume of stools or gases, you may not be able to "hold 'em." This particular mechanism is behind the action of the rectal enemas, glycerin suppositories, and most laxatives.
Just like any other muscle, both anal sphincters may become too tense and interfere with orderly bowel movement by constraining the diameter of the anal canal. Chronic stress, conscious stool withdrawals, the bouts of diarrhea, and habitual flatus retention may lead to the over-tensing of the anal sphincters, further exacerbating constipation, straining and related complications.
The nerves of the anus and rectum are highly sensitive, and particularly so in children. For this reason, children's ability to resist encroaching bowel movements and/or gases is not as strong as in adults, who are much more practiced at this art. So if your child has had a faux pas, don't scream at or shame her, otherwise you'll make her too self-conscious, too controlling and, soon, too constipated and prone to straining in order to overcome her "insensitive" anus or overly constrained anal canal.
Hydro-C — the formula that I developed to specifically overcome (among other things) pediatric stool withdrawals and the excessive tension of the anal sphincter in adults works so effectively by rapidly building up the intra-rectal pressure and stimulating nerve receptors of the anus to the point of no-resistance, and ensuing complete relaxation.
The aperture of the relaxed anal canal in adult human is 35 mm (1.4") slightly larger than an American quarter ($0.25 coin). If your stools become larger than that, you need to strain to expel them.
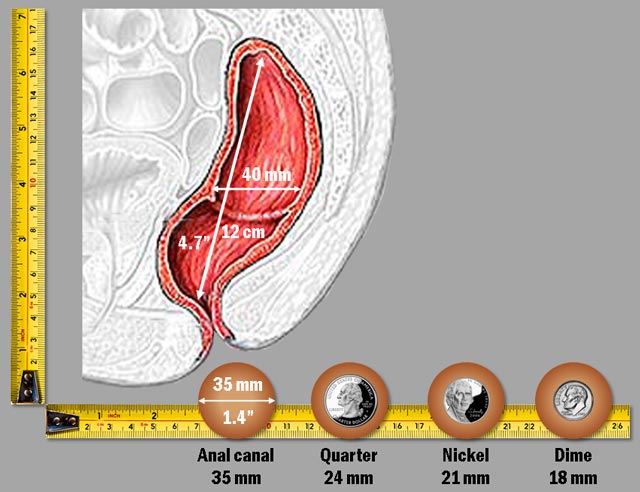
A scale comparison of the adult rectum and anus aperture to the dimensions of common coins.
The anal canal expands to 35 mm without apparent harm when there are no enlarged internal hemorrhoids to constrict it. Anything beyond that size is bound to cause pain. If an individual is tense, he or she may not be able to completely relax the external anal muscle, and may experience pain even from smaller stools.
Technically, your fist is about the same size as your fully stretched mouth. Try to swallow your fist to get an idea what your anus feels like when your stools grow larger than normal size.
To give you even a better idea of just how "jammed up" these quarters are, take a look at the next illustration. It compares a Q-tip with an anatomical cross-section of the anus and rectum. Keep in mind that the proportions on all of these illustrations are 1:1. Obviously, they look smaller on the screen, so you may want to look at an actual Q-tip to get a better sense of the real sizes:
The anal canal is small, tight, vulnerable, not easily repairable, and... indispensable. So, take good care of it from the get-go unless you don't mind a "little hemorrhoids" here and there for the rest of your life.
That is how small and tight the human rectum, anus, and anal canal really are. Much smaller than you may think looking at your behind in the mirror. You can learn all that and much more from any anatomy book:
"The Rectum is about 12 cm. long [...] The Anal Canal [...] measures from 2.5 to 4 cm. in length." [Gray's Anatomy]
Thus, for truly effortless passing even without enlarged hemorrhoids, the stools must be soft, moist, light, and no larger than a nickel coin or one's middle finger (15-20 mm) on this illustration:
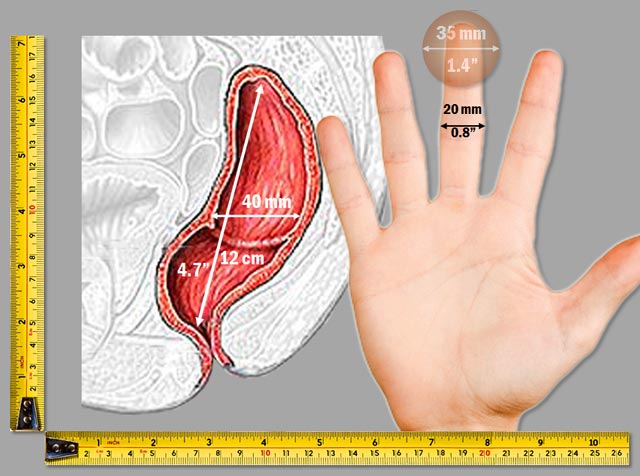
If you don't wish to develop enlarged hemorrhoids or anal fissures in the near future, make sure your stools aren't larger than your index finger.
These kind of picture-perfect, finger-sized, soft and moist stools require no more effort to pass out than urination. In other words, normal defecation is a practically unnoticeable act, just like it was when you were a healthy child.
On the other hand, if the stools are large, let's use a pickle — something we can both relate to without looking at the "real thing" — to compare its size with the anus. As you can see even a smallish Corby pickle is huge relative to the anus size. And not just the anus — the pickle is about the same size as the entire rectum.
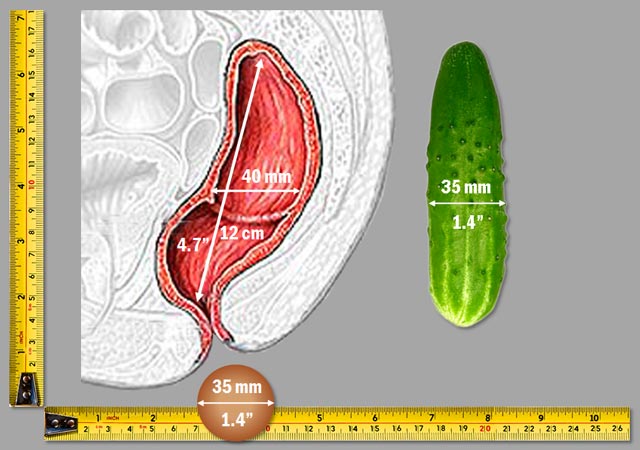
This is how the large stools look like relative to your anal canal, although, of course, not as appetizing as on this picture.
So, if anyone is telling you to "eat more fiber" to "bulk up" your stools, so you can relieve or prevent hemorrhoidal disease and anal fissures, give that person a Corby pickle, and ask him or her to jam it up their anuses, and, then, tell you how normal it feels. If that experience does not get them out of the pickle you got yourself into with painful hemorrhoids or bleeding fissure, nothing will...
All that said, the anus can still pass stools larger than that pickle. It doesn't have a choice, does it? But it wasn't intended to do so regularly, in the same way your teeth weren't intended to open beer bottles, even though they can.
Not surprisingly, when the anus is overstretched by large stools, the forces needed to pass them — pressure from the inside, straining from the outside — cause hemorrhoids to enlarge or skin to tear up, and this brief passage to the sewer gradually becomes one long tortuous journey.
How torturous? Based on the U.S. Census 2010, — half of the population — by age fifty translates into over 40 million victims of hemorrhoidal disease. Once you factor in people under fifty and the undiagnosed, the actual number is probably even greater.
What giveth? Newton's third law, of course: for every action there is an equal and opposite reaction. Here's what I mean:
- As hemorrhoids get larger, the anal canal aperture gets smaller, and the stools become harder to pass;
- As the difficulty of passing stools intensifies, the need to strain grows more pronounced, and the hemorrhoidal pathologies turn worse;
- As the first two problems evolve, people often keep increasing the amount of dietary and/or supplemental fiber to counteract defecation difficulties;
- As people increase the amount of fiber in their diet, their stool keep getting larger, causing further enlargement of hemorrhoids, while the anal aperture becomes smaller and smaller;
- As the anal aperture becomes smaller and the stools larger, people experience more constipation, strain harder, feel more pain, and begin experiencing anal fissures and other complications described elsewhere on this site and in my books.
If this chain of events isn't interrupted by luck, education, or God's will, the vicious cycle continues unabated until patients require surgery to fix rectal prolapse, anal fissures, fistulas, abscesses, fecal incontinence, or other related ailments.
Because most surgeries leave scars, damage nerves, and affect surrounding tissues, recovery is rarely one hundred percent. The muscle damage alone may place you in diapers for the rest of your life because of fecal incontinence. The residual pain may cause incomplete or delayed stools — the culprits behind chronic fecal impaction with its own compliment of nasty ills, such as diverticular disease, irritable bowel syndrome, ulcerative colitis, precancerous polyps, and, to top it off, colorectal cancer itself.
No, I am not making all this up. Here is what proctologists — the physicians who specialize in mending hemorrhoids — have to say about the unfolding of hemorrhoidal disease: "Unfortunately a hemorrhoidal condition only tends to get worse over the years, NEVER better [link]"
That is certainly true if you continue treating hemorrhoidal disease with evermore fiber, water, laxatives, and exercise. Otherwise, never say never!
It may surprise you to learn that every individual on planet Earth possesses hemorrhoids since birth. It's true, because hemorrhoids aren't what you think they are. What you think they are, is, in fact, hemorrhoidal disease, not hemorrhoids. What's the difference?
Well, hemorrhoids (plural) are the internal bundles of vascular, muscular, and connective soft tissue that lines the anal canal and the region around the anus. The three main bundles (also referred to as anal cushions) encircle the anal canal, and some minor ones are situated in between. A ligament connects each sponge-like bundle to the underlying muscle, and the mucous membrane protects them from above.
Just like all other organs, hemorrhoids develop while still in the womb. They are part and parcel of human anatomy, not a pathology or disease. Their function is to protect (cushion) the internal structures of the anal canal from the passing stools. They are almost like the bearings on which the stools ride.
To some degree the function (and dysfunction) of hemorrhoids is similar to calluses that protect joints from friction damage. And, just as calluses on your palms can bulge, blister, and bleed as the result of too much hard labor, so can hemorrhoids from large stools and straining. No surprise there.
The term hemorrhoid (singular) means the condition, the sum of symptoms related to the inflammation, enlargement, thrombosis, and/or prolapse of hemorrhoids (tissue bundles). Doctors and patients alike universally refer to hemorrhoidal disease as hemorrhoids, which is technically incorrect. That's why this chapter refers to hemorrhoidal disease throughout, rather than hemorrhoids.
The two types of hemorrhoids are distinguished anatomically — internal and external. While the external hemorrhoids are innervated by the same nerves that supply the skin in the perianal region, the internal hemorrhoids aren't innervated at all and do not cause pain, even when enlarged. Let us be grateful to Mother Nature for small mercies!
Enlarged internal hemorrhoids are detected in two-thirds of all patients during routine anorectal examinations [link]. The absence of innervations explains why so many people with a history of straining may not realize that they have irreversible hemorrhoidal disease, until suddenly confronted with hemorrhoidal bleeding or prolapsed hemorrhoids.
In the case of external hemorrhoidal disease, the pain emanates primarily from the inflammation of the skin protruded by dilated hemorrhoidal veins, by the venal thrombosis, or both. The external dilation (that can be seen or felt) is caused by venal thrombosis. The thrombosis is caused by a blood clot (thrombus).
Usually, the clotting happens from a specific event that cause venal obstruction. It may be the passing of large stools, intense straining, the lifting of heavy objects, hard labor, diarrhea, childbearing, anal intercourse, or similar actions.
The vein's altered shape causes skin folds (tags) which may protrude temporarily (after defecation) or permanently. The hemorrhoidal dilation reduces after blood clot dissolves and the affected vein shrinks, though rarely completely.
That's when secondary conditions, such as poor perianal hygiene, prolonged sitting or standing, an alcoholic binge, smoking, a hot bath, sauna or the like, trigger events that may cause a recurrence of another clot, protrusion, and/or skin inflammation.
Unlike external hemorrhoids, internal hemorrhoids cause pain indirectly. The pain is precipitated by rectal prolapse (the protrusion of internal hemorrhoids outside the anus), while the following conditions cause actual pain:
- The spasm of the anal sphincter complex caused by the prolapsed hemorrhoids.
- The strangulation of the prolapsed hemorrhoidal tissue.
- The inflammation of the perianal skin caused by the residue of mucus and fecal matter, supplied by prolapsed tissue.
- The spasm of the anal sphincter may cause the thrombosis of underlining hemorrhoidal veins, which in turn may cause new external hemorrhoids, or aggravate existing ones.
- The anal fissure related to straining and narrowing of the anal canal [from enlarged internal hemorrhoids].
To prevent a possible necrosis of strangulated hemorrhoidal tissue, an affected individual must seek immediate medical attention. When it isn't available, the prolapsed hemorrhoids should be returned back into the anal canal in order to relieve pain and prevent possible necrosis and infection. The affected area must be cleansed with warm water, which also helps to relax the anal sphincter. Petroleum jelly or non-medicated hemorrhoidal cream should be used to lubricate prolapsed hemorrhoids and the surrounding area before maneuvering them back inside the anal canal.
Taking care of bloody business
Bleeding specific to hemorrhoidal disease isn't usually from the thrombosed veins (another popular misconception), but from the abrasions, cuts, fissures, fistulas, or ulcerations of the mucosal membrane that lines the anal canal.
Hemorrhoidal bleedings are distinguished by crimson streaks of fresh blood on the passing stools. The stool itself doesn't change color, because there was no prior contact between feces and the laceration.
The bleeding related to ulcers, polyps, and tumors in the colon and the rectum may look identical to hemorrhoids-related bleedings. The appearance of mucus along with the blood is a telltale sign of inflammatory bowel disease or colorectal tumor(s). So any time you see blood, mucus, or both in the toilet bowl or on the toilet paper, get checked immediately.
If the stool's appearance is already tar-like, it may mean that there is internal bleeding at some point upstream, beginning from the esophagus. The color changes to tar after coagulated blood mixes with feces.
At times, the bleeding may be profuse, but it usually stops when defecation is completed. In any event, it is best to see a doctor to rule out ulcers or tumors in close proximity to the rectum.
The mucosal membrane that lines the anal canal is quite resilient and infection-proof. It quickly heals, and will not bleed again as long as stools remain soft and small (BSF type 5 or 6). If the stools remain type 1 to 4 (lumpy, large, hard), or you strain while relieving yourself, the bleeding may continue and get worse.
In those instances, an initial small abrasion may turn into a fissure (split that won't heal), a fistula (duct from anus into perianal region), or an abscess (encapsulated pus) — conditions that, considering the location and "traffic," are extremely painful, infection-prone, and hard to treat and heal.
Keep this important point in mind: if blood emanates from upper intestinal tract organs (esophagus, stomach, duodenum, small intestine), the bleeding may have started at least 24 hours before you see the first signs of it. That's how long it normally takes for chyme to turn into stool and reach the toilet bowl. For people who are severely constipated it may take even longer. This means that by the time the blood in stools is detected, the loss of blood may be considerable.
Certain food (beets, blueberries, black licorice, black coffee, dark chocolate), supplements (dietary iron), antacids (Pepto-Bismol), or a sudden release of conjugated biliary salts may also give stools a tar-like appearance.
Instead of panicking, don't flush the toilet and run to the nearest drugstore to purchase a Fecal Occult Blood Test (FOBT) kit. Even better — purchase one on Amazon in advance, and keep it on hand just in case. The "occult" in the FOBT means hidden, not mystic.
To regain your piece of mind, follow the instructions provided with the kit — usually a strip of paper that you'll drop into the toilet — to observe changes. If the test is positive, and your pulse rate happens to be high, your blood pressure low, your appearance pale or you find that you're short of breath, fatigued or dizzy, you should call 911 at once. These are all symptoms of serious blood loss.
If you feel fine, get to the nearest emergency room ASAP, and advise the triage nurse that you've just had a positive FOBT. They'll know what to look for next. Don't waste precious time seeing your local doctor, because you'll be sent to the nearest hospital anyway, and, in the meantime, could be losing equally precious blood. Just make sure to refuse abdominal CT scan citing concerns over radiation exposure, a risk of allergy to contrast solution, claustrophobia, or any other plausible excuse to avoid making an already bad situation even worse [link].
I assume that you recognize the importance of visually inspecting your stools at every opportunity. Besides saving yourself a lot of grief, it may actually save your life. In many cases, the toilet bowl predicts your future with more certainty than a crystal ball.
Hemorrhoidal disease is grouped into four categories — from the 1st degree, which is the least serious, to the 4th degree, which usually requires surgery. Repeatedly prolapsing internal hemorrhoids are commonly treated by nonoperative methods, such as rubber band ligation, sclerotherapy, cryoterapy, photocoagulation, laser ablation, and others.
Surgical treatments are reserved for the more complex cases (usually 4th degree). Recurring external hemorrhoids are treated by surgical excision of the overlying skin folds and underlying veins. The procedure is performed under local anesthetic, and usually on an outpatient basis.
The consensus among surgeons who specialize in treating anorectal disorders is that asymptomatic enlarged hemorrhoids are better off left alone, and that the conservative treatment — thorough hygiene, prevention of diarrhea and constipation, avoidance of known triggers, and soft, small, and regular stools that don't require straining to expel — is the safest, most reliable approach.
The medical profession is also in universal agreement that straining (related either to diarrhea or constipation) and large stools (type 2 and 3) are the primary reasons behind recurring prolapses of internal and/or external hemorrhoids. In other words, to prevent and treat hemorrhoidal disease you must have small, soft, regular stools and you must not strain.
Living with hemorrhoidal disease
Unfortunately, you can't reverse the damage already caused by large stools and straining — the dilated hemorrhoidal veins, the enlarged internal hemorrhoids, and the skin folds around the anus.
Fortunately, you may reduce the severity and progression of hemorrhoidal disease, anal fissures, and related complications simply by reducing the size and hardness of feces, and by eliminating straining as described on this page and on the rest of this site.
These two common sense actions — reducing the size and/or hardness of stools and eliminating straining — are all that is needed to turn a major pain in the butt into a minor inconvenience in cases of early to mid-stage hemorrhoidal disease or anal fissures. This is irrespective of other causes, be it natural child birth, severe diarrhea, anal intercourse, weight lifting, occupational hazards, or some others.
Following the recommendations below, you can prevent your veins from getting dilated further, and your hemorrhoids from becoming larger and protruding even more. In most cases that's enough to stop pain, inflammation, bleeding, or prolapse, and keep it that way for as long as you guard your anus with the same vigilance you guard your credit rating.
Same steps apply to the prevention and healing of the anal fissures because both conditions are interrelated. Here is how:
Step #1. Eliminate dietary fiber
Considering fiber's impact on stool size, you must first eliminate dietary fiber and fiber laxatives from your diet! There are three key properties of fiber — bulk, acidity, and gases (the last two from fermentation) — that make it such a disastrous choice for those living with hemorrhoidal disease:
-
Bulk. Large stools require straining to expel them. Once your anal canal becomes obstructed by the enlarged hemorrhoids, you must strain harder and harder. The harder you strain, the more the obstruction of the anal canal increases from further enlargement of the hemorrhoids.
And so it goes until one day you end up with prolapsed internal hemorrhoids, screaming from pain and oozing blood. To make matters words, the straining related to internal hemorrhoids, begins to cause external hemorrhoids as well, bringing its own set of on-going headaches.
To make this point loud and clear, let me remind you again that the most debilitating hemorrhoids-related conditions, such as torture-like pain and the inability to sit or walk, aren't related to internal hemorrhoids, but external.
-
Acidity. The colon's environment is mildly alkaline. The continuous acidity from fiber's fermentation causes mucosal inflammation, decimates desirable bacteria, and provides a good breeding ground for infectious bacteria inside the colon.
Adding insult to injury, the acidity can cause even more pain and itching of the already inflamed mucosal membrane of the anal canal or the skin folds in the perianal area caused by external hemorrhoids.
The first problem — the pain and itching inside the anal canal — causes intermittent urges to defecate and the sensation of incomplete emptying. This, in turn, stimulates a strong straining reflex to suppress the urge sensation again and again, with all the "crap" that follows, particularly for external hemorrhoids.
The second problem — the chemical irritation of the outer skin around the anus — causes additional inflammation and mind-bending pain that we associated with external "hemorrhoids."
-
Gases (flatulence). The gases create permanent pressure inside the colon and contribute to straining, sometimes intense, to suppress them, particularly when at work or in social settings. So, in addition to all the other indignities related to flatus, you can also add the inevitable enlargement of internal and external hemorrhoids.
To eliminate fiber dependence, follow my recommendations in the Overcoming Fiber Dependence guide.
Step #2. Restore intestinal flora
Healthy bacteria reside and procreate inside the protective layer of the mucosal membrane, and derive their nutrients from mucus. To give them a good home and head start, your mucosal membrane must be healthy, well-nourished, and populated with beneficial bacteria. To accomplish this goal, follow my recommendations in the Dysbacteriosis (Dysbiosis) guide.
Step #3. Eliminate straining
Straining is a "side effect" of large stools, hard stools, irritable bowel syndrome, anorectal nerve damage, impaired peristalsis, and constipation.
Whatever you happen to have, all of these conditions are addressed in depth in the Restoring Normal Bowel Movements and Restoring Anorectal Sensitivity guides. If you are affected by IBS, please also study the Irritable Bowel Syndrome guide.
It goes without saying, that all of these guides are interrelated, and all three steps are usually executed in parallel.
In case of sharp pain while moving bowels, a skin inflammation, or a confirmed rectal bleeding related to anal fissure or hemorrhoids — study the Hydro-CM program's page and use it to normalize your condition. Once you are stable, return to the Step#1 above to avoid the redux of the same emergency again and again.
Summary: Mind over fecal matter
To prevent hemorrhoidal disease from disfiguring your anus, consider the following key points:
- Hemorrhoids are an intrinsic part of human anatomy. They protect the internal structures of the anal canal (muscles, vessels, tissues) from passing stools.
- There are two type of hemorrhoids — external and internal. They are distinguished by their location and innervation.
- Hemorrhoids enlarge from internal pressure caused by large and/or hard stools, and external pressure caused by straining.
- Anal fissures are caused by the same mechanical forces that lead to the enlargement of the internal hemorrhoids.
- Enlarged internal hemorrhoids increase the likelihood of anal fissures because they narrow the aperture of the anal canal and require more effort (i.e. straining) to expel stools.
- Internal hemorrhoids do not cause pain, unless they prolapse outside the anus.
- The prolapse of internal hemorrhoids is caused primarily by large stools and extreme straining specific to late-stage latent and organic constipation.
- The prolapse of external hemorrhoids is caused by the dilation and thrombosis of hemorrhoidal veins.
- External hemorrhoids cause pain, the sensation of which is related to inflammation of the skin that surrounds the thrombosed venal prolapse.
- Other conditions cause hemorrhoidal disease indirectly, by either applying pressure similar to the passing of large stools — such as during anal intercourse, or straining during pregnancy and bouts of diarrhea — or through the lifting of heavy objects.
- Enlarged hemorrhoids are a chronic but benign condition. Hemorrhoidal disease is an acute recurring condition, characterized by inflammation, pain, and/or bleeding of affected tissues.
- The enlargement of hemorrhoids narrows the aperture of the anal canal. This contributes to the development of constipation, larger stools, and further damage.
- Type 1, 2 or 3 stools (hard and/or large) on the BSF scale cause hemorrhoidal disease and anal fissures because their dimensions exceed the anatomical "specification" of the anal canal.
- Any stools above 2.5 cm (1") in width are likely to cause the enlargement of hemorrhoids. To prevent hemorrhoids from enlarging, stools must match type 4 to 6 on the BSF scale.
- Dietary fiber is an indirect cause of hemorrhoidal disease and anal fissures, because it causes large stools.
- The elimination of dietary fiber (to reduce stool size and density) from the diet is a principal strategy for the treatment and prevention of hemorrhoidal disease and related complications.
- The commonly accepted recommendation to use dietary fiber for the treatment and prevention of hemorrhoidal disease or anal fissures is grossly incorrect. Dietary fiber will aggravate enlarged hemorrhoids and prevent the healing of anal fissures, because increased stool size causes additional pressure inside the anal canal.
- The appearance of blood on passing stools indicates a laceration of the anal mucosa that covers internal hemorrhoids. The blood may appear without any visible symptoms of hemorrhoidal disease. Consult your doctor at once to diagnose the source of bleeding, and to eliminate all other probable causes.
- Asymptomatic enlarged hemorrhoids do not require any treatment except dietary modification (exclusion of fiber), and the maintenance of small, soft stools, which don't require straining.
- If, or when, hemorrhoidal disease impacts your quality of life, or prevents you from having timely, regular stools because of pain, fear, or other factors, discuss more proactive treatment options with a specialist.
- Even though most GI physicians are qualified to perform outpatient surgeries related to hemorrhoidal diseases, choose a doctor who specializes exclusively in anorectal surgeries. There is no substitute for experience when dealing with this delicate area.
- There are many surgical and non-surgical methods to treat hemorrhoidal disease and anal fissures. Some are safer than others. Always ask your doctor about his or her approach, and investigate its pros and cons to avoid common complications such as chronic pain or fecal incontinence.
- If hemorrhoidal disease or anal fissures are left untreated, and their causes aren't eliminated, there is a distinct possibility of further anorectal complications such as fistulas, and abscesses, which in most cases require surgical intervention.
- If you are experiencing an acute stage of hemorrhoidal disease, follow your doctor's directions until the symptoms subside. Do not drop prescribed medication or recommended laxatives, unless you successfully replace them by the safer means, methods, and approaches recommended on this site.
- Hemorrhoidal disease is inevitable for as long as you heed irrational medical advice to consume more fiber, drink more water, and strengthen abdominal muscles in order to move bowels. To remain hemorrhoids-free throughout your entire life, follow the recommendations on this site, and teach your children to move bowels as soon as they sense an urge, usually during or shortly after a meal.
***
Medicines that may cause large and/or hard stools:
The list below is far from being comprehensive. Any drug that affects the functions of muscles, nerves, neurotransmitters, electrolytes, digestive and endocrine functions, and other bodily functions has a potential for enlargement and/or hardening of stools. In general, these medicines will have constipation and/or diarrhea listed as one of their side effects:
Depression, anxiety, and mood disorders: Amitriptyline, Doxepin HCI, Amitriptyline (Elavil), Trimipramine (Surmontil), Doxepin (Sinequan), Desipramine (Norpramin), Nortriptyline (Pamelor), Protriptyline (Vivactil), St. John’s Wort;
Treatment of psychosis: Haloperidol, Pianozide, Risperidone, Thiothixene, Olanzapine, Clozapine, Chlorpromazine, Thioridazine;
Hypertension, prostate disorders, glaucome: Calcium-channel blockers, Clonidine (Catapres), Clonidine/Chlorthalidone;
Antiarrhythmic drugs: Disopyramide, Verapamil;
Parkinson’s disease: Bromocriptine, Trihexyphenidyl (Artane), Benztropine mesylate (Cogentin), Biperiden (Akineton), Procyclidine (Kemadrin);
Elevated cholesterol: Cholestyramine, statins (Lipitor, Mevacor, Zocor, and others);
Peptic ulcer: Sucralfate;
Cough remedies with opioids: Hydrocodone bitartrate, Chlorpheniramine polistirex, Hydrocodone tartrate, Homatropine methylbromide;
Anti-inflammation and anti-rheumatic drugs: Sulindac (Clinoril), Ketoprofen (Orudis);
Diarrhea: Loperamide hydrochloride (Imodium);
Pain medication: Acetaminophen & codeine, Fentanyl, Hydrocodone, Hydromorphone, Meperidine, Methadone, Morphine/ Morphine sulfate, Oxycodone, Oxymorphone, Propoxyphene, Tramadol;
To screen out any medication that you may be taking, please visit Drugs.com, RxList.com, or WebMD.com and review prescription information for your particular medication. If it has constipation and/or diarrhea listed as one of their side effects, it may contribute to the progression of hemorrhoidal disease and/or cause anal fissures due to large and/or hard stools. Do not abandon any medication without consulting first with your healhtcare provider [back].
What are conjugated biliary salts?
The conjugated biliary salts form in the gallbladder from bile, and are the precursors of gallbladder stones. Fat-free or low-fat diets and obstruction of the duct that connects the gallbladder to the duodenum contribute to formation of gallstones. The obstruction itself may be caused by salts, stones, inflammation, or a combination of all three.
The actual release of salts may be sudden, without any apparent reason, or preceded by a specific event, such as an airplane flight, certain foods, or medication. Apparently, the changes in atmospheric pressure or some other factors may cause the release of biliary salts during or after the flight.
When the released salts reach the large intestine, they cause profuse stools or diarrhea because of their strong laxative effect. People may often confuse this condition with "travelers" diarrhea, since it isn't described in medial literature [back].