Why is fiber such a menace to your health?
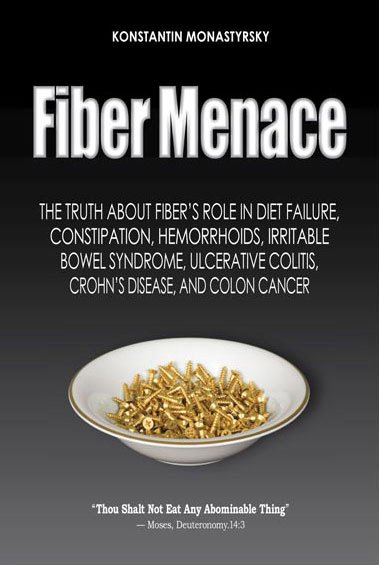
Fiber Menace: The Truth About the Leading Role of Fiber in Diet Failure, Constipation, Hemorrhoids, Irritable Bowel Syndrome, Ulcerative Colitis, Crohn's Disease, and Colon Cancer.
You might be surprised to find out that the original intent behind fiber consumption wasn‘t the betterment of your health, but the suppression of sexuality! As this book explains, fiber has indeed succeeded at rendering a great many men and women sexually dysfunctional.
That's why just a generation ago, avoiding fiber was the quintessence of prudent nutrition. Caring parents everywhere, American and European alike, were earnestly peeling fruits (apples, peaches, pears, prunes) and skinning vegetables (tomatoes, peppers, eggplant, potatoes) before giving them to children or eating them themselves.
The French and Italians still do it. And the Japanese diet is practically fiber-free. Americans, on the other hand, are urged to consume 30 to 40 grams of dietary fiber daily, regardless of their age and health.
Many heed this advice (some with a vengeance), assuming there can‘t be too much of a good thing. The outcome is predictable: a pandemic of digestive disorders, diabetes, heart disease, cancers, and obesity. These problems are worse in the United States than in any other Western country.
All this seems hard to believe until you actually begin examining the role of fiber in human nutrition, Thus, the point of Fiber Menace isn't telling you what to eat, but what not to eat and why. Here is a chapter-by-chapter summary of what's under the cover along with a sprinkle of readers' reviews (full names are omitted for medical privacy reasons):
Introduction: Thou Shalt Not Eat Any Abominable Thing
Fiber Madness or Madness from Fiber. While studying the history of Japanese cuisine, I came across a remarkable historical fact: in the name of Buddhism, which postulates strict vegetarianism, the Samurai class prohibited ordinary Japanese citizens from hunting, fishing, and keeping livestock. Their reasons were quite instructive, especially for anyone wanting to be as robust and as healthy as a proverbial "Samurai:" [Read Introduction]
Part I. Truth, More Truth, and Diet Failure
Chapter 1, Fiber Carnage describes the role fiber plays in both nutrition and disease, in layman‘s terms. It concludes that fiber is an addictive substance, meaning that after you begin consuming fiber specifically for its “health benefits,” you‘ll need more and more fiber with every passing year to get, literally, the same “kick in the ass.” If you abuse any organ too long and too hard, it eventually breaks down. The list of fiber-related fault lines is so long, the chapter takes over thirty pages just to describe the major ones. [Read Chapter 1]
Thinking out of the box — this book is pricelessI would love to tell you how this book has helped me with my daughter. She is 20 years old and has severe cerebral palsy, full care, and in a wheel chair. […] TRULY A MIRACLE. SHE IS BASICALLY FREE FROM ALL THE HORRIBLE SYMPTOMS except for very occasional constipation which is not a nightmare anymore. SHE IS SLEEPING THROUGH THE NIGHT FOR THE FIRST TIME IN 20 YEARS. M.A.C., New Jersey
Chapter 2, Water Damage explains why the widespread popularity of fiber brought with it another menace: increased consumption of water. Not because more water is actually needed, but because the advice to “eat more fiber” invariably accompanies the advice to “drink more water.” Water is every bit as addictive as fiber, but for a different reason—the more you drink, the more you urinate, the more you urinate, the more water you need to replace it. Unfortunately, you don‘t urinate just water. Urine washes out minerals that are crucial for health, especially potassium. Potassium deficiency happens to be one of the primary causes of costiveness (hard stools) and constipation (irregular stools). When that situation arises, you‘ll be advised to increase fiber and water consumption. Imagine what happens next. [Read Chapter 2]
Fiber Menace & my experience with fiberIn the last five months, while making a point of cutting down on fiber and excess water consumption, I have lost 31 pounds and my HDL [healthy] cholesterol has also gone up somewhat, which puts it in the high range. My cardiac risk ratio has gone down significantly as my CRP test [c-reactive protein] showing heart inflammation is also down quite a bit. L.M., Colorado
Chapter 3, Atkins Goes to South Beach illustrates the connections between fiber and obesity, and fiber and diet failure—two of the most pressing public health problems of our generation. The Public health authorities‘ incessant urging that we consume more natural fiber in the form of bread, pasta, cereals, fruits, and vegetables is precipitating an obesity epidemic, because fiber-rich foods contain ten to twenty times as much carbohydrate as they do fiber (5% to 10%). Unfortunately, by the time you‘re ready to jump on the low-carb bandwagon, dropping carbs cold turkey doesn‘t work, because your colon is already dependent on fiber to move your bowels. If you throw the shortcomings of the Atkins and South Beach diets into this mix, you end up with diet failure. If you didn‘t get major anorectal damage from the “hard landing,” consider yourself lucky. For anyone who aspires to lose weight and preserve health, this chapter alone makes reading this book worthwhile. [Read Chapter 3]
To eat or not to eat: that is the questionIf you ever pondered a question why you can't lose weight, look no further. This book is your answer. With the true mastery, K. Monastyrsky "walks" his readers through the basics of the elegant process of weight loss. "Fiber Menace" is a jewel and a real eye opener. It is clever, informative, well researched and entertaining. Enjoy! O.H. Ohio
Part II. All the Proof You Need
Chapter 4, Dysbacteriosis. At one point or another, anyone may experience costiveness (large, hard stools, need to strain) or constipation (irregular stools regardless of size, shape, and volume). There are many reasons behind these conditions (also known as dysbiosis), ranging from bad parenting to bad poisoning, from too much fiber to too little fat, and everything in between. Whenever external factors compromise bowel movements, the normal bacteria inside the large intestine are the first to suffer. Because these bacteria make up the bulk of normal stools (up to 75%), once they‘re gone, stools harden up because the bacteria are no longer there to retain water, soften the stools, and provide “bulk.” This chapter describes the sorry travails of these hard-working little bugs, deciphers the events that precede their demise, and explains their connection to health, longevity, and disease. [Order on Amazon]
Fiber MenaceA fabulously informative book for those seeking knowledge on how to achieve optimal digestive function, and a must read for those interested in the repair and recovery of the entire GI system. As a person who suffers from chronic constipation I found the author's advice extremely effective and perhaps even life saving. I have resolved much of the suffering I encountered and have improved by about 90%. I continue to use the recommended recovery supplements, eat a healthy tasty diet, and am free of all fiber supplements which I had used for many years. The author's writing is clear, easy to read, thorough, and even fun for the delicate topic of digestion and elimination. There is plenty of room to tailor the program to one's specific needs or preferences. G.S.
Chapter 5, Constipation. After the bacteria are gone, fiber enters the picture to replace their function. For a while, it may even work as advertised. Fiber makes stools voluminous and not as hard, and the problems appear to be gone. Unfortunately, this is merely the calm before a calamity: “normality” comes not from restoring the body‘s natural clockwork, but from replacing it with an outside bulking agent; essentially, a laxative. For a while, the problems are hidden because you don‘t yet feel them. This chapter describes the transition through the three phases of fiber-dependence that accompanies the functional (reversible), latent (hidden), and organic (irreversible, only manageable) stages of constipation. [Order on Amazon]
Child safe - child helpedThe information in this book is solid, easy to read, and practical. It can be implemented, as our family did implement it. I am grateful because my daughter no longer struggles with constipation on an ongoing basis. [...] This works. Don't be discouraged -- there is hope. Signed as Gracious Mom
Chapter 6, Hemorrhoidal Disease. Here comes the reckoning: large stools [caused by fiber] and the straining needed to expel them wear out and damage the small, taut and extremely delicate anal canal. Enlarged hemorrhoids are the first signs of trouble. As hemorrhoids get larger, the anal canal opening gets smaller, and constipation gets worse. When that happens, most people add more fiber to their diets. Naturally, the stools get even larger, the anal canal opening even smaller, and the constipation more severe than ever. This chapter describes the role of fiber in the pathogenesis and evolution of this disorder, which afflicts up to half of all adult Americans by the age of 50. That‘s close to the number of people who become overweight on high-carb, high-fiber diets. What goes around, comes around. [Order on Amazon]
Life saverThe beauty and strength of this book is that the approach is rational and makes no exaggerated claims. You are given a very detailed description of the process of digestion and elimination, and a highly informative account of how the process can be disturbed by over use of fiber. In my case it was a revelation.B.L., CA
Chapter 7, Diverticular Disease. As we get older, the muscles, bones, eyes, and hearing all grow weaker. The large intestine is no exception. By the age of 60 up to half of all Americans are affected by diverticular disease, which is an irreversible bulging of the large intestine. There is only one force that can make the intestinal walls bulge out: large stools. There is only one food component that causes large stools: dietary fiber. This chapter explains why this happens, what you can do to prevent it, or how to make the condition benign if you already have it. Trust me, you don‘t want to experience the complications. [Order on Amazon]
You need this bookI read Fiber Menace in one day and immediately began cutting out all the foods he'd suggested be cut. It took about 48 excruciating hours to transition from a woman whose intestines felt as if they were about to burst (mucosal inflammation, extreme anxiety from not being able to crap, sore rear-end, the whole nine yards) to a relaxed woman whose bowel movements come twice daily with no effort. I've lost several pounds, my stomach is flatter, and I'm eating foods I truly enjoy. Needless to say, I cannot recommend this book enough. Signed as Melissa
Chapter 8, Irritable Bowel Syndrome. The combined impact of dysbacteriosis, a fiber-rich diet, laxatives, constipation, and hemorrhoids (not necessarily all of them or in that order), brings along yet another torment—irritable bowel syndrome. It is a functional condition, which means that it‘s completely reversible. The problem is that everyone tries to reverse it with more fiber and more drugs, rather than with less fiber and bacterial supplements. This chapter explains why up to 60 million Americans “can‘t get no relief,” and how so many of them set themselves up for what‘s addressed in Chapter 9. [Order on Amazon]
IBC-C victimAt the young age of 21 I was struck down by IBS-C [constipation-dominant]. I'm 22 years old at the pinnacle of health due to Fiber Menace. This book is more like a Bible. It has kept my life from shambles when the doctors sent me around town to specialists which resulted in more fiber and less hope.A.F.
Chapter 9, Ulcerative Colitis and Crohn‘s Disease. These two diseases are considered irreversible, points of no return. Sure they are, as long as they‘re treated with even more fiber, even more antibiotics, even more immunodepressants, even more antispasmodics, and even more laxatives. After you finish reading this chapter, you, too, will be scratching your head in disbelief. If, God forbid, you suffer from one of these conditions, you‘ll know what to do to turn back the tide. If you do nothing, ulcerative colitis increases the chances of getting colorectal cancer by “32 times the normal rate” according to the National Institutes of Health. That‘s, believe it or not, 3,200%. [Order on Amazon]
A must... if you really care for your health...
It will change your life!Well is hard to even put in words how incredible my life turned around after I really applied all the knowledge I got from reading this book. […] I strongly recommend that you read every word in the book (including footnotes—there is no waste—and maybe not only once) because it will open your eyes regarding why so many digestive problems nowadays...H.E., New York
Chapter 10, Colon Cancer. Think about it: according to this book, dietary fiber is the primary cause of ulcerative colitis. Ulcerative colitis increases the chances of getting colon cancer a great many times over. To prevent colon cancer, you‘re being told to consume more fiber. Well, hope springs eternal, as they say. This chapter reviews recent research data that tells the unwelcome truth: fiber does little or nothing to prevent colon cancer, and may actually contribute to colon cancer. This research doesn‘t come from the bowels of the Internet, but from some of the most distinguished medical publications and establishments out there, such as The Lancet, The New England Journal of Medicine, Centers for Disease Control and Prevention, The National Cancer Institute, The World Health Organization, and the like. [Order on Amazon]
Top book to fix constipationI am so happy I found Konstantin Monastyrsky's website and book. I searched for information about constipation on the Internet for a few days before I stumbled on to the website by chance. I am very grateful that he researched all these topics so thoroughly. I applied the principles he set out and I noticed the changes IMMEDIATELY. My bowel habit improved remarkably. Fixing the constipation has brought about other improvements in my health. (Signed as Reader Critic)
Part III. From High To Low Without a Blow
Chapter 11, Avoiding the Perils of Transition. Imagine the promise of spectacular and permanent weight loss, and then the disappointment experienced among people who failed on the Atkins or South Beach diets because of constipation, indigestion, hypoglycemia, dehydration, and other “side effects” of reduced fiber diets. This book can malign fiber all it wants, but what good will it do if fiber addiction can‘t be broken without these debilitating conditions? This chapter explains the causes behind the fallout from fiber withdrawal, and describes key strategies for a crash-free transition from a high- to low-fiber lifestyle. This brings us to the final chapter. [Order on Amazon]
Open you mind to open your bowelThis book is Great, It's Easy to read and very entertaining. All the references check out and you begin to ask why this isn't common knowledge. The book is worth reading just to know how much water to drink, let alone all the great ideas regarding constipation and help with the GUT. All of which work perfectly. I recommend the book to all. it helped me help my daughter and many friends too. J.A., United Kingdom
Chapter 12, The Low-Fiber Advantage. Humans are extremely vulnerable to just about anything out of the ordinary: heat, cold, fire, smoke, darkness, slippery surfaces, and so on. The natural, innate fear of trauma and death keeps most of us away from these types of perils. Not so with health—as a rule, most people don‘t value it until they no longer have it. Inversely, the value of health becomes palpable when we first begin experiencing diseases, especially those that cause pain or defy a quick fix. This chapter enumerates the key benefits of excising fiber from your diet. These benefits range from weight loss and improved digestion to recovery from diabetes, indigestion, irritable bowel syndrome, Crohn‘s disease, and ulcerative colitis—disorders that defy conventional treatment because drugs can only sugarcoat their symptoms, but can do nothing to remove their causes. Fiber is the champion of harm among these conditions. [Order on Amazon]
A bit of common sense and the world is your oyster!I find this book absolutely invaluable - finally! Somebody showed with simplicity and solid logic what fiber and water can do to your body and eventually to your life and career! Having Master's in Science I can assure that the principles described in the book do have a great deal of logic. Having an MBA degree I can assure you that this book was by far the best investment of my life - my health is what I really value! Get "Fiber Menace", read it, think about it, work on it - and believe me - the world is yours! M.J, Virginia
Frequently Asked Questions
Q. Give me ten reasons why I should read Fiber Menace.
Q. Is this book really for me, and not my doctor? What if I am okay?
Q. Does this site rehash the information in your book?
Q. But what if you are still dead wrong about fiber?
Q. Why isn't my doctor telling me about your approach if it is so simple and effective?
Q. But I am still scared to get off fiber. What should I do?
Q. I am confused about what I should eat...
 “My training as a physician included many hours of nutrition, but fiber was only mentioned in regards to the effects of a deficiency. Never once did any of my professors consider the possibility that too much of what has always been considered a good thing' could have such harmful or far-reaching consequences. The author's detailed description of the trauma imposed to the gastrointestinal mucosa by the expanding fiber is a vivid reminder that returning to the basics of GI function and logically thinking through what our bodies actually are designed to do with the food we eat, should be the first step on anyone's journey to recovery from digestive disorders. Thanks to the insights in this book I have slowly begun to change my approach to common patient symptoms, which I traditionally would have treated by suggesting increased fiber and more water to correct! So far the results are promising.” Dr. John Turner, DC, CCSP, DIBCN
“My training as a physician included many hours of nutrition, but fiber was only mentioned in regards to the effects of a deficiency. Never once did any of my professors consider the possibility that too much of what has always been considered a good thing' could have such harmful or far-reaching consequences. The author's detailed description of the trauma imposed to the gastrointestinal mucosa by the expanding fiber is a vivid reminder that returning to the basics of GI function and logically thinking through what our bodies actually are designed to do with the food we eat, should be the first step on anyone's journey to recovery from digestive disorders. Thanks to the insights in this book I have slowly begun to change my approach to common patient symptoms, which I traditionally would have treated by suggesting increased fiber and more water to correct! So far the results are promising.” Dr. John Turner, DC, CCSP, DIBCN
March 2, 2007
[link]
Reality check: The Stats Behind Fiber's Disaster
Even if I wanted to, I couldn't dream up the number of digestive disorders affecting Americans in my worst nightmares. Unfortunately, it's all too true. No wonder we have the costliest healthcare system in the world. Here are some facts from the back cover:

The epidemiological statistics cited on the back cover was obtained from the following sources:
1. Every tenth adult American (over 21 million*) has been diagnosed with an ulcer at least once in his or her lifetime.
Number of noninstitutionalized adults with diagnosed ulcers: 14.5 million” “Percent of noninstitutionalized adults with diagnosed ulcers: 6.8%
Centers for
Disease Control and Prevention
Summary Health Statistics for U.S. Adults, 2003, tables 7,
8;
2. Every fifth American (up to 60 million*) suffers from irritable bowel syndrome.
In fact, irritable bowel syndrome (IBS) affects approximately 10-20% [30 to 60 million – ed.] of the general population.
About Irritable Bowel Syndrome (IBS);
International Foundation for Functional Gastrointestinal
Disorders;
3. Every second adult over age fifty (about 38 million*) is affected by hemorrhoidal disease.
Hemorrhoids are very common in both men and women. About half of the population have hemorrhoids by age 50.
National Digestive Diseases Information Clearinghouse,
a service of the National Institutes of Health;
Hemorrhoids; NIH Publication No. 02–3021; Feb. 2002;
4. Every second adult over age sixty (about 23 million*) suffers from diverticular disease.
About half of all people over the age of 60 have diverticulosis.
National Digestive Diseases Information Clearinghouse,
a service of the National Institutes of Health
Diverticulosis and Diverticulitis; NIH Publication
No. 04–1163; 4/04
5. Depending on who‘s counting, over 80 million* Americans endure chronic constipation.
The exact prevalence of constipation depends on the definition used; prevalence estimates range from 2% to 28%.
Talley NJ; Definitions, epidemiology,
and impact of chronic constipation;
Rev Gastroenterol Disord. 2004;4
Suppl 2:S3-S10. PMID: 15184814;
6. Besides impaired digestion, over 137 million* adult Americans are overweight or obese…
Results from the 1999-2002 National Health and Nutrition Examination Survey (NHANES), using measured heights and weights, indicate that an estimated 65 percent of U.S. adults [over age 20 – ed] are either overweight or obese.
Centers for Disease Control
and Prevention
Prevalence of Overweight and Obesity Among Adults:
United States, 1999-2002;
*To calculate population breakdown:
U.S. Census 2000; Age Groups and Sex: 2000
As you can see, fiber's toll on our health is huge. On a purely statistical level, fiber causes more harm and death than tobacco, alcohol, and illicit drugs combined.
Not surprisingly, just as in the case of the tobacco industry, those who benefit most from peddling fiber will keep squeezing every penny of profit out of it for as long as they can weasel their way around the truth.
And why not? Baking cereals from cattle chow (bran), or making laxatives from chicken feed (psyllium) is as profitable as minting money. No, probably more profitable!
Another aspect of this tragedy is even scarier. Just as tobacco keeps a substantial slice of the medical industry gainfully employed, patching up fiber's shenanigans makes it rich. So why stop the windfall?
YOU MUST READ THIS BOOK. Read with an open mind & consider, just consider, the possibility of trying something totally new with your diet to change around your symptoms & bring gut healing. My desperation was so bad I was willing to try anything, and it was that open attitude that lead me to healing through the methods in this book. Good luck. M.K, Chicago
Fortunately, there is hope. This is an institutional problem, not a professional one. The absolute majority of honest, hard-working, and honorable doctors, nurses, pharmacists, nutritionists, and dietitians are as victimized by fiber-related deception as their patients.
So while I am critical of many aspects of medicine, it doesn't imply that I am critical of medical professionals wholesale. Just like you can't blame a soldier for carrying out his generals' orders, you can't blame individual doctors for abiding by established guidelines.
Once, when I was presenting a lecture on a related subject, one lady in the audience got up and said:
— Mr. Monastyrsky, what you are saying irks me, but, as a physician, I can't find a single flaw with it.”
If ever I need a doctor, I'd like to be treated by an introspective and honest doctor just like her. This excerpt from Fiber Menace represents some even more nuanced discussions of this complicated subject.
So, if you want change, please, point out this site to medical professionals in your life, or give Fiber Menace to read to your physician or pediatrician. That's how the change will come—one good doctor at a time!
Konstantin Monastyrsky
I started suffering from constipation around age 16. Despite being so young and athletic, I was also always bloated, fatigued, and depressed. Stumbled across GutSense.org at the age of 19. After reading Fiber Menace, I cut out fiber out of my diet, and not only did I lose weight, but also regained unlimited energy and easier bowel movements.
I must also say that a low fiber diet actually decreases my appetite! The book is correct in the fact that too much fiber stretches out the stomach, and you have more appetite. Most amazing, I didn't even have to change the way I eat dramatically. I still consume bread, cereals, pasta. I just eat the refined versions that have little to no fiber.
I work out and engage into intense exercise 4 times a week, and need carbohydrates to fuel my active lifestyle. My workouts feel much better after switching to a low fiber diet. And this proves that fiber can destroy the digestive health of certain people. I can still consume lots of bread and dairy, and feel fine. The only thing I changed about my diet, was reducing the fiber!
Konstantin's book is a life saver and a true masterpiece. His supplement's, including Hydro-C, are also worth every penny. They are natural, and offer the best results.V.C. (via e-mail)