Part I. The Anatomy Of A Deadly Deception
Colorectal cancer is one of the most dominant and the deadliest nutrition-related cancer — close to one hundred sixty thousand new cases diagnosed annually in the United States alone. [1]
So our desire to prevent it isn't surprising, especially when we are told that regular colonoscopies after age fifty make colorectal cancer "more than 90% curable — but only if you get tested in time." [2]
Actually, this is a lie! Screening colonoscopies do not prevent or materially reduce anyone's risk of colorectal cancer regardless of age. And if anything, they may actually increase your overall risk of cancer, and not just colorectal.
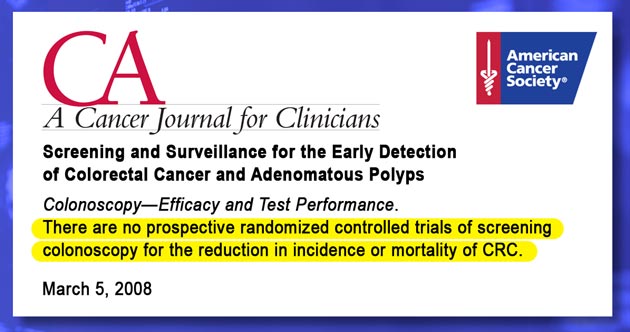
First, according to the American Cancer Society, up till now… “…There are no prospective randomized controlled trials of screening colonoscopy for the reduction in incidence or mortality of colorectal cancer.” [3]
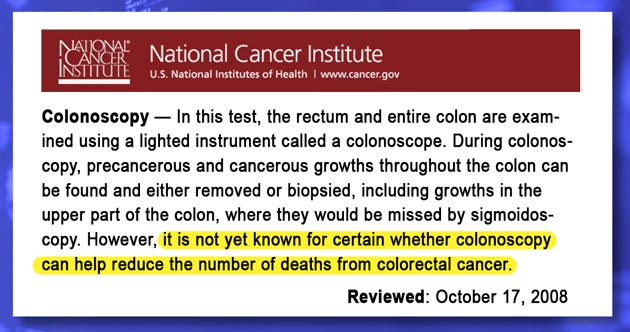
The National Cancer Institute is even more explicit:“…it is not yet known for certain whether colonoscopy can help reduce the number of deaths from colorectal cancer.” [4]
This means that the 90% cure rate figure cited by Ms. Couric back in 2000 is pure fiction. It also means that most of the fourteen million plus screening colonoscopies [5] performed annually in the United States to the tune of twenty to thirty billion dollars aren't recommended on the basis of rock-solid research or clinical indications, but on the willful misinformation of the American public, consumer fraud in other words…
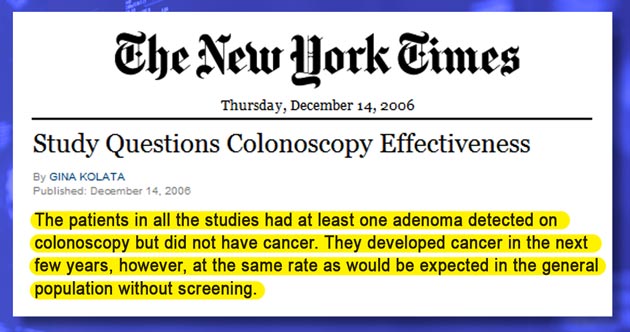
Second, according to the analysis of actual outcomes, ‘screening colonoscopies’ are essentially useless: “The patients in all the studies had at least one adenoma detected on colonoscopy but did not have cancer. They developed cancer in the next few years, however, at the same rate as would be expected in the general population without screening.” [6]
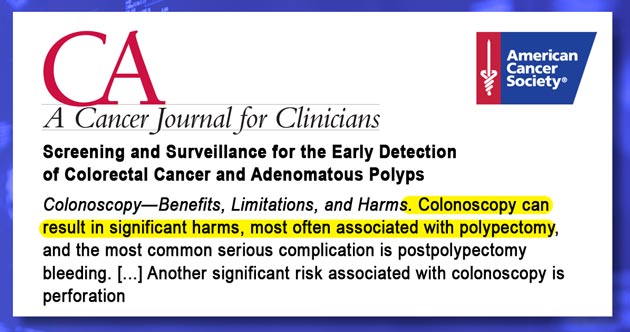
Third, colonoscopies aren't as safe and simple as you may think or are led to believe: “Colonoscopy can result in significant harms, most often associated with polypectomy, and the most common serious complication is post-polypectomy bleeding”, and “Another significant risk associated with colonoscopy is perforation,” of the colon, that is... [3]
And that is even before taking into account your stress, anxiety, false positives, frequently missed polyps and tumors [7], and all of the usual recovery-related complications, such as infections, constipation, diarrhea, hemorrhoids, diverticulitis, and others.
But all these risks pale in comparison with 'computed tomography,' known as virtual colonoscopies. Incredulously, instead of preventing your risk of cancer, they actually increase it by exposing you to five to ten millisieverts of x-ray radiation required for just one abdominal scan.
According to the United States Food and Drug Administration... "This range is not much less than the lowest doses of five to twenty millisieverts received by some of the Japanese survivors of the atomic bombs." [8]
Goodness gracious... Radiation levels from a single virtual colonoscopy are similar to the atomic bomb exposure in Hiroshima, even though, according to The National Cancer Institute: “Whether virtual colonoscopy can reduce the number of deaths from colorectal cancer is not yet known.” [4]
But the really frightening part comes next: "This increase in the possibility of a fatal cancer from radiation can be compared to the natural incidence of fatal cancer in the U.S. population, about 1 chance in 5." [8]
Not surprisingly, the actual incidence of colorectal cancers in the United States has grown by 30,000 more cases annually, a whopping 22% increase in just eight short years. (The incidence of colorectal cancers in the United States has increased from an estimated 129,400 new cases in 1999 [10] to 158,410 in year 2007 [11, page 4].)
Author's commentary: Someone sent me a rather nasty comment suggesting that this increase in the incidence of colorectal cancer demonstrates the success of colonoscopies in detecting and treating early cancers. It very well maybe true. There are, however, four serious problems with this argument:
— First off, the patients are urged to undergo screening colonoscopies to PREVENT colon cancer occurrence with 90% certainty, not to DETECT early colon cancer. For that, you can take a safe, simple, and more economical FIT- or blood test as often as you like, and without incurring any risk of either getting killed or injured by colonoscopy, or missing a cancer in progress. And I recommend that much in part II for anyone with propensity for hypochondria.
— Second, early detection of asymptomatic colorectal cancer may actually shorten patient's life, because it automatically triggers inevitable biopsy, surgery, and chemotherapy. Otherwise it takes about 10 years for most colorectal tumors to become symptomatic (i.e. large enough to cause problems that requires surgical intervention).
— Third, if you get operated on for a two year-old asymptomatic tumor, your chances of premature death are far greater than if you get operated on for a ten year old tumor eight years later. And you get to live about the same age-adjusted lifespan after the treatment. Thus, doing nothing buys you at least an extra eight years of normal life and care-free bliss!
— Fourth, there is greater than 95% chance that you will succumb to any other terminal disease or old age before colorectal cancer has a chance to kill you, while any attempt to eliminate that 5% risk of colorectal cancer with screening colonoscopies increases your cumulative risk of death far greater than 5%. To learn why, please watch parts III and IV.
So ask yourself this simple question: would you rather take a 5% chance of dying from a large colorectal tumor eight years from now; or undergo surgery and chemo today, wear a colectomy bag for the next eight years, and most likely die anyway before eight years are up from some other cancer, stroke, or heart attack caused by post-treatment complications?
In terms of cancer, this sharp upsurge is considered an epidemic of catastrophic proportions. So why, then, do doctors recommend colonoscopies if they are unproven, ineffective, risky, and unreliable?
Because colonoscopies generate enormous income for a small group of specialists. In 2010, total annual revenue from colonoscopy procedures in the U.S. was estimated at $10 to $12 billion. At the time, there were only about 11,000 practicing gastroenterologists performing most of these procedures, which translates to roughly $900,000 to $1.1 million in annual revenue per physician for colonoscopies alone. This concentrated financial incentive helps explain the aggressive promotion of colonoscopy, even in cases where the clinical benefit is questionable.
Doctors‘ profit motives aside, Katie Couric isn't exactly a benevolent Samaritan either. She began urging Americans to get screened for colon cancer while she was being employed by General Electric, the owner of NBC television.
GE happens to manufacture and sell CT scanners used for virtual colonoscopies. Since each of these room-sized contraptions [link] costs upward of three-and-a-half million dollars, what is a better way to keep them 'minting money' than an indirect endorsement by a big TV star.
Lo and behold, her handlers ruthlessly exploited her husband's unfortunate death from colon cancer to promote colonoscopies. Because Ms. Couric never disclosed her connection to GE Healthcare — a seventeen billion dollar subsidiary of GE and a sister company of NBC [link] — unsuspecting Americans embraced her story, and the number of screenings jumped from under one million before her famous televised colonoscopy in year 2000 to around fourteen million in 2009.
Adding to this hypocrisy, Jay Monahan - Ms. Couric's late husband - passed away at age forty two, eight years before a first screening is even recommended. This, unfortunately, means that neither him nor anyone else in his predicament would have likely been saved…
Based on all the above evidence, I pleaded with Mr. Couric first by mail [link], second on her blog [link], and finally on my site, to stop endorsing or recommending colon cancer screening to 95% of Americans, who are in a low-risk group. Regretfully, she ignored my pleas and never responded.
One change I noticed… After Ms. Couric left NBC for greener pastures at CBS, she no longer refers to the 90% cure rate [link]. Now, it is just a measly 5% reduction of "colon cancer death."
Katie Couric: “Colon cancer is the second leading cancer killer. But if it is detected early, it has better than 90% cure rate.” (from 2000, [link])
And seven years later…
Katie Couric: "Colon cancer death are down almost 5% among men, and 4.5 among women." (from 2007, [link])
Sadly, even this small reduction isn't likely related to screenings, and I discuss its probable reasons [link] on this video's transcript page.
After this report had already been published, the Annals of Internal Medicine — a preeminent publication of the American College of Physicians — released a new research paper concerning the considerable failure of screening colonoscopies to detect and prevent colorectal cancer, particularly in the right colon.
The editorial commentary by Dr. David Ransohoff, the Professor of Medicine at the University of North Carolina at Chapel Hill, states the following [12]:
“A goal of avoiding all deaths from colon cancer may be admirable, but we do not have evidence that we can achieve it.”
“Although colonoscopy is generally safe, it is still an invasive procedure with a 0.2% rate of serious complications —10 times higher than for any other commonly used, cancer-screening test. Repeated examinations over time may incur a substantial cumulative rate of complications, not even counting hard-to-detect complications (if they occur), such as silent myocardial infarction [heart attack — KM].”
“Colonoscopy is an effective intervention, but, as Baxter and colleagues suggest, we must realize that current evidence is indirect and does not support a claim of 90% effectiveness.”
— So, who, then, should get screened for colon cancer, if anyone?
You‘ll find the answer to this question in the second part of this investigative report.
Author's commentary: After reading the above section, you may ask yourself this completely sensible question:
— How can a scornful Ms. Couric claim a 90% reduction of colon cancer risk while an indignant Konstantin claims no reduction, only an increase?
Oh, that's easy… Just like a horse race, any clinical study can be easily fixed to deliver the desired outcome either by falsifying the trial design, or by manipulating outcome statistics, or both. That's how this 90% figure came about, and until this day I can't locate the original sourcing for this figure.
From this point on, these scams are managed using well-learned and well-practiced formula:
- By using cherry-picked references from prestigious medical journals. The articles in many of these journals aren't generally available to the general public, so it's easy to obscure undesirable outcomes and conclusions;
- By donating money to not-for-profit associations, whose sole function is to promote their donors. The National Colorectal Cancer Research Alliance was co-founded by Katie Couric specifically for this purpose — to funnel “blood money” to promote screening colonoscopies.
- By hiring so-called “expert spokespersons” who will endorse and champion anyone willing to pay up, and so on.
And this obfuscation was particularly easy to accomplish in cases of screening colonoscopies, because, unlike drugs, medical equipment, or lab tests, the diagnostic protocols do not, I repeat, do not require anyone's approval or oversight.
As far as my indignation goes, once you too realize that screening colonoscopy can't reduce anyone's risk of colon cancer for the same fundamental reasons you can't crossbreed a cat with a dog, you'll no longer question it.
References
Click the [link] to view the source site or document in the new window (when available). The references for this essay were compiled in December 2008 —February 2009. Some of the links may not match at a later date because publishers may revise their web sites. In this case, try searching cached pages on Google, or contact the respective publishers.
1American Cancer Society. Cancer Facts & Figures 2007. Atlanta: American Cancer Society; 2007. [link]
2The National Colorectal Cancer Research Alliance, Don't end up saying "if only." Get tested." [link]
3Levin, B., at al.; Screening and Surveillance for the Early Detection of Colorectal Cancer and Adenomatous Polyps, 2008: A Joint Guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology CA Cancer J Clin 2008 58: 130-160 [link]
4Colorectal Cancer Screening; National Cancer Institute; Oct 2008; [link]
5Seeff LC, et al.; How many endoscopies are performed for colorectal cancer screening? Results from CDC's survey of endoscopic capacity. Gastroenterology. 2004;127: 1670-1677. [link]
6Study Questions Colonoscopy Effectiveness; The New York Times; G. Colata; Dec 14, 2006; [link]
7Barclay, R., at al.; Colonoscopic Withdrawal Times and Adenoma Detection during Screening Colonoscopy N Engl J Med 2006 355: 2533-2541
8What are the Radiation Risks From CT?; U.S. Food and Drug Administration; Center For Devices and Radiological Health; August 6th,2008; [link]
9Jerry M. Cuttler; What Becomes of Nuclear Risk Assessment in Light of Radiation Hormesis? Proceedings of the 25th Annual Conference of the Canadian Nuclear Society, Toronto, June 6-9, 2004 [link, Word document]
10Rudy, D, et al.; Update on Colorectal Cancer; American Family Physician; March 15, 2000; [link]
11Cancer Facts & Figures, 2007; Atlanta: American Cancer Society; 2007, page 4 [link]
12Ransohoff, D.; How Much Does Colonoscopy Reduce Colon Cancer Mortality? Ann Intern Med 2008; 60520-308. [link]
The following references apply to the to other sources mentioned throughout this section:
— Complications of Colonoscopy in an Integrated Health Care Delivery System; T. R. Levin, W. Zhao, C. Conell, L. C. Seeff, D. L. Manninen, J. A. Shapiro and J. Schulman; Ann Intern Med 2006; 880-886. [link]
— Virtual Colonoscopy Misses Nearl One Third of Lesions; The proceeds of the 68th annual scientific meeting of the American College of Gastroenterology; Oct 15, 2003; [link]
— Association of Colonoscopy and Death From Colorectal Cancer; N. N. Baxter, M. A. Goldwasser, L. F. Paszat, R. Saskin, D. R. Urbach and L. Rabeneck; Ann Intern Med 2009; 1-8; [link]
— Screening and Surveillance for the Early Detection of Colorectal Cancer and Adenomatous Polyps, 2008: A Joint Guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology; Levin, Bernard, at al; CA Cancer J Clin 2008 58: 130-160; [link]
— The Effect of Fecal Occult-Blood Screening on the Incidence of Colorectal Cancer; Mandel, Jack S., Church, Timothy R., Bond, John H., Ederer, Fred, Geisser, Mindy S., Mongin, Steven J., Snover, Dale C., Schuman, Leonard M.; N Engl J Med 2000 343: 1603-1607; [link]
— Population-based surveillance by colonoscopy: effect on the incidence of colorectal cancer. Telemark Polyp Study I.; Thiis-Evensen E, Hoff GS, Sauar J, Langmark F, Majak BM, Vatn MH.; Scand J Gastroenterol. 1999 Apr;34(4):414-20; [link]
— Colorectal Cancer Risk Assessment Tool; National Cancer Institute; [link]
